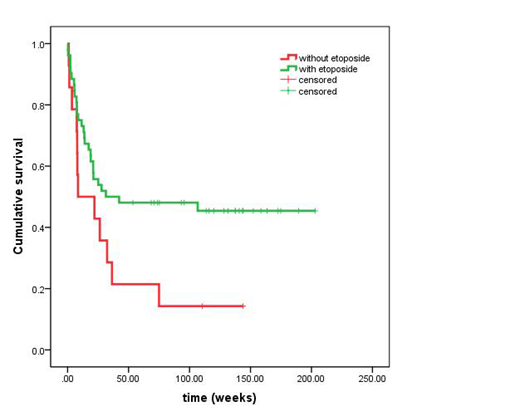
Background: Hemophagocytic lymphohistiocytosis (HLH) is a severe or even fatal inflammatory status caused by a hereditary or acquired immunoregulatory abnormality. It is divided into two categories: primary and secondary. Secondary HLH (sHLH) is often associated with and caused by infections, malignant tumors, and autoimmune diseases. Lymphoma associated HLH (LAHS) is one of the most common sHLH, usually presents worse prognosis higher mortality. The treatment strategy for LAHS is still controversial. Etoposide is one of the key drug in HLH-94/04 regimen. We sought to identify the importance of including etoposide in the initial treatment of LAHS, especially comparing with the high dose chemotherapy. Methods: The patients diagnosed as LAHS in our center between Jan 1 2015 and Dec 31 2017 were observed. Survival times were calculated from the date of diagnosis of HLH. All patients were followed up until death or 31 Dec 2018, whichever occurred first. Patients undergoing stem cell transplantation were censored on the date of that procedure. Results: There were 68 patients in total. The median age of the patients was 48 years (15-76 years). They were divided into two groups according to weather the initial treatment containing etoposide. There were 53 patients with initial etoposide and 15 without it. The baseline level between two group shows no differences (p>0.05). The treatment regimens with initial etoposide include HLH-94/04 regimen, DEP (doxorubicin-etoposide-methylprednisolone), L-DEP (PEG-aspargase and DEP regimen), E-CHOP (etoposide and CHOP regimen) and RE-CHOP; those without the initial etoposide, but high-dose chemotherapy, include CHOP/COP, R-CHOP/COP, L-CHOP, CVAD, L-GDP regimen and et al. The response rates of the 68 patients was 66.1%, with the CR rate of 25% (17/68) and PR rate of 41.1% (28/68). A total of 32 cases with initial etoposide achieved remission, and the remission rate was 71.7% (CR 28.3% and PR 43.4%). 7 cases with chemotherapy without etoposide achieved remission, and the remission rate was 46.7%. A significant difference was noted between the two groups (p<0.01). A total of 41 deaths occurred with a total mortality rate of 60.3%. There were 28 deaths in patients with initial etoposide (mortality rate 52.8%) and 13 deaths in the other group (mortality rate 86.6%). A significant difference in mortality was noted between the two groups (p=0.020). Comparing the long-time survival between two groups, the survival of the initial etoposide group (101w±13, 95%CI [76, 127]) is significantly better than that of the no initial etoposide group(37w±12.7, 95% CI [12.0, 61.9]) (p=0.43) (Figure 1). Conclusion: As one of the secondary HLHs, LAHS suffers the worst outcome among all the types of HLH. This study found that initial treatment including etoposide, comparing with the chemotherapy without etoposide, can provide higher response rate, lower mortality rate and better survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal