Introduction:
Large granular lymphocyte (LGL) leukemia is a rare lymphoproliferative disorder characterized by clonal expansion of cytotoxic T-lymphocytes or natural killer (NK) cells. It typically has an indolent course with most patients eventually needing treatment as it is associated with severe cytopenias, recurrent infections and autoimmune conditions. While the main goal of treatment is the relief of symptoms and includes using immunosuppressive agents, there is no standard therapy established due to lack of prospective clinical trials due to its relative rarity. Furthermore, currently there are no curative treatment options for LGL leukemia. We sought to describe the frequency of associated manifestations, response to treatment and clinical course of the patients with LGL leukemia.
Methods:
All adult patients (age >18 years) diagnosed with LGL leukemia at University of Arkansas for Medical Sciences over a period of 11 years (from 2007 to 2017), were identified using retrospective chart review. We identified patient characteristics including demographics, clinical features, associated malignancies and autoimmune conditions, laboratory results, treatment modalities and therapy outcomes.
Results:
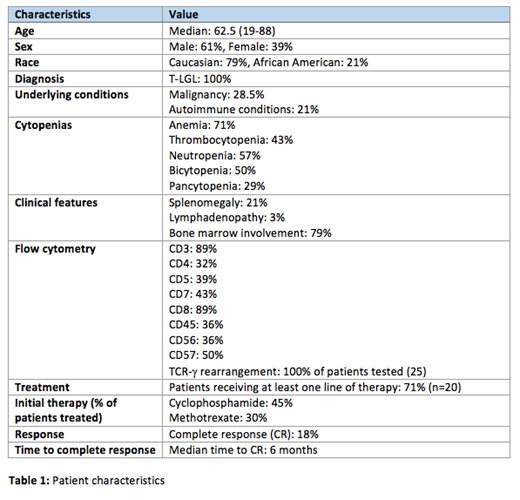
A total of 28 patients with LGL leukemia were identified. All 28 patients were diagnosed with T-cell LGL leukemia. Median age of patients was 62.5 years (range: 19-88 years). 61% of patients were male and 39% were female. Out of the 28 patients, 79% were Caucasian and 21% were African-American. 8 (28.5%) patients had associated malignancies, most common of which was MDS (n=3), followed by breast cancer (n=2), and 1 each of multiple myeloma (MM), acute myeloid leukemia (AML), and liposarcoma. 6 (21%) patients were found to have associated autoimmune disorders, with rheumatoid arthritis (n=2) and ITP (n=2) being the most common, along with psoriasis (n=1) and aplastic anemia (n=1). Anemia was common, seen in 71% of patients (n=20), thrombocytopenia in 43% (n=12) and absolute neutropenia in 57% (n=16) of patients. Bicytopenia was noted in 50% of patients and 28.5% of patients presented with pancytopenia. Lymphocyte count ranged from 0.54-5.81 x10^9/L with a median of 2.63 x10^9/L, and LGL count ranged from 0.19-6.3 x10^9/L with a median of 1.21 x10^9/L. Splenomegaly was seen in 6 patients (21%) and lymphadenopathy was rare with only 1 case reported. Bone marrow involvement was noted in 79% of patients (n=22). Flow cytometry results were as follows, with presence of the following markers: CD3: 89%, CD4: 32%, CD5: 39%, CD7: 43%, CD8: 89%, CD45: 36%, CD56: 36%, CD57: 50%. TCR-γ rearrangement was performed in 25 patients and was positive in 100% of patients tested. 20 patients received some form of therapy, out of which initial therapy was most commonly with cyclophosphamide (45%) and 30% patients received oral methotrexate. Other initial therapies included Daratumumab/Velcade, Alemtuzumab, Fludaribine.
Complete response was seen in only 18% of patients (n=5) after initial therapy, 3 of whom had been treated with Cyclophosphamide initially. Median time to response in those with complete response was 6 months. No relapses were noted in those with complete response. Second line therapies for those who experienced partial response (n=4) or progression (n=5) included cyclosporine (n=2), cyclophosphamide (n=3) and methotrexate (n=3). No LGL leukemia related deaths were reported in the study population.
Conclusions:
In this retrospective study, we described LGL leukemia associated manifestations and clinical course. Despite the indolent nature of this disease, majority of our patients required treatment due to associated symptoms. However, we were able to achieve complete response in less than 20% of the patients. There is a definite need for new therapeutic options.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal