Introduction: Loss of heterozygosity (LOH) was described for many malignancies including leukemia. Using chromosomal microarray analysis (CMA) we have shown preliminary (Risinskaya et al. HemaSphere, 2019, V.3, No S1, P.782) that LOH in STR loci in tumor cells with the normal karyotype represents the loss of extended chromosomal areas and could be associated with uniparental disomy of the entire chromosomal arm or the entire chromosome. Uniparental disomy results not only in the elimination of the wild type allele, but also may lead to the duplication of the mutant allele of certain candidate tumor gene(s). Retrospective analysis of archival samples have shown that in most cases STR loci absent at the relapse of disease were already lost at the onset of disease. We noted LOH at STR loci is especially frequent for relapsed ALL patients and could be used as prognostic factor for possible poor clinical outcome.
The aim: To identify LOH in the blast cells of the patients with ALL at the onset of disease and to analyze therapy outcome relative to the patients without LOH. We expect LOH in the de novo ALL to be an unfavorable factor, and those patients possibly should be treated like high-risk group.
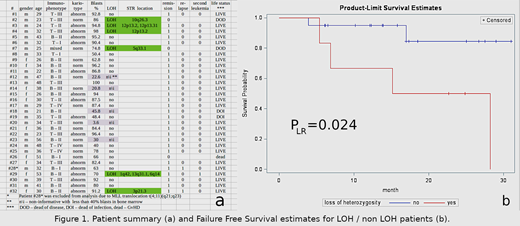
Patients and Methods: This study includes a comparative analysis of the STR profiles of the DNA of tumor and normal cells from bone marrow samples on a cohort of 32 patients with de novo diagnosed Ph-negative ALL undergoing treatment according to the "RALL-2016" regimen at the National Research Center for Hematology (Moscow, Russia). Inclusion criteria: de novo diagnosed Ph-negative acute lymphoblastic leukemia (ALL) patients, 18-55 years old, intermediate risk group without MLL translocation t(4;11)(q21;q23), treatment by RALL-2016 protocol. Exclusion criteria: other diagnosis, adult patients older than 55 years, MLL translocation t(4;11)(q21;q23), pretreatment or treatment by other protocol. The presence of blast cells in bone marrow samples was confirmed morphologically. DNA was isolated from patient bone marrow samples taken at different disease stages. Control DNA samples were taken from blood of patients in complete remission and/or from buccal epithelium (buccal swab). STR-profiles were assessed by PCR with COrDIS Plus multiplex kit for amplification of 19 polymorphic STR-markers and amelogenin loci (Gordiz Ltd, Russia). The fragment analysis was performed on ABI3130 Genetic Analyzer. The data processing was accomplished using GeneMapper v.4-0 software. A multivariate survival analysis was used to assess the independent impact of the LOH as risk factor against the background of the abnormal tumor karyotype as standard factor for this cohort of patients. We have chosen Failure Free Survival (FFS) as primary endpoint for short-time follow-up and small patient sample size. Death from any reasons, relapse and second leukemia were chosen as failure events, survival time interval starts from begin of treatment. SAS V9/4 was used for statistical analysis of the data.
Results: Of the 32 patients six were found with LOH in the certain STR loci (19%). Of these six, two were resistant to therapy and died from disease progression. One patient with LOH is currently in relapse and one patient with multiple LOH has a second leukemia (Fig.1a). Only two from six patients are "Failure Free" now, whereas only three patients from 26 in group without LOH died (two from infectious complications and one from GvHD after BMT). P value < 0,05 (Fig.1b).
Conclusions: We have found statistically significant association of clinical failures with the LOH in STR loci measured at the onset of ALL. We assume that LOH is an unfavorable prognostic factor for de novo ALL patients and could be used for risk stratification and choice of adequate therapy implying allogeneic hematopoietic stem cells transplantation or modern innovative therapy approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal