
Background
During the last five decades the life expectancy for people living with sickle cell disease (SCD) has improved markedly, with median survival of 61 years in recent cohorts enrolled from academic centers. Older adults with SCD (defined herein as age ≥ 50 years) make up 13% of the adult population at four major academic medical health systems in North and South Carolina. As this population continues to grow, more data are needed to guide medical management appropriate to their needs, as a lifetime of vaso-occlusion often leads to functional decline and premature development of complications seen in geriatric populations. There are no validated assessment tools and interventions to improve physical function in older adults with SCD. In this study we evaluated the feasibility of a focused geriatric assessment (FGA) for older adults with SCD.
Methods
Twenty adults with SCD ≥ 50 years old were enrolled in a prospective cohort study. Measures previously validated in the oncology FGA were included and enriched with additional physical and cognitive functional measures. Activity monitoring was performed for 7 days using the Actigraph wT3X-BT, and biomarkers were collected at each study visit (baseline, 10-20 days after a hospitalization [for those who experienced a hospitalization during the study period] and 12-month after baseline). The primary endpoint was the proportion of subjects who complete the assessment. Secondary endpoints were duration of the FGA, proportion who completed the activity monitoring and lab collection, and acceptability.
Results
Twenty-one of 25 older adults approached for the study consented. Nearly all (20/21, 95%) completed the FGA. One was removed after missed study visits. The median duration of the assessment was 97 minutes (range 73-175 minutes), and there were no adverse events. The mean age was 57 years (range 50-71), 50% (10) were female, 30% (6) were on disability and 50% (10) were working. 45% (9) were former smokers but only 5% (1) were current smokers (Table).
On the acceptability survey, 95% (19) reported the length of the assessment as appropriate. 10% (2) subjects reported a portion of the Montreal Cognitive Assessment (MoCA) as difficult. No subject found the questions upsetting, and 2 subjects reported that they would remove redundant questions.
All subjects had a Karnofsky Performance Score of at least 80% and were able to complete activities of daily living. A third (35%) had been admitted in the last 6 months, and most (75%) had had severe pain crises at home that limited their activity. 40% (8) had > 4 severe crises at home in the last 6 months.
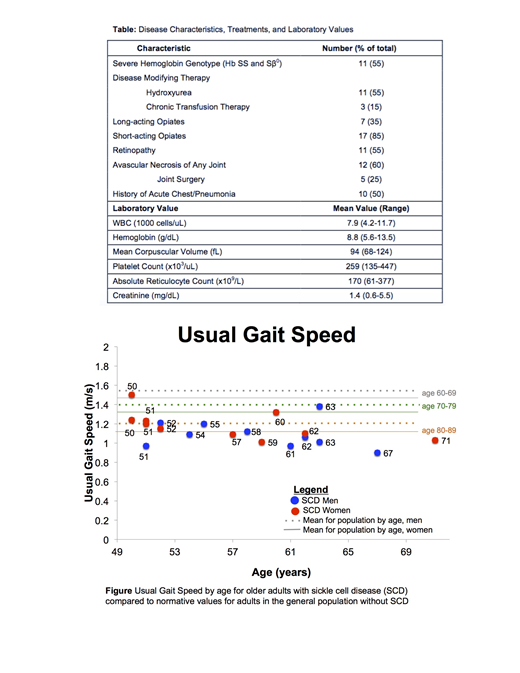
The mean usual gait speed was 1.14 m/sec (range 0.90-1.50) (Figure). Mean Timed Up and Go (TUG) was 10.1 seconds (range 7.7-14.0). Two (10%) subjects had a TUG consistent with increased fall risk (≥ 12 seconds). Mean grip strength of the dominant hand was 39 kg (range 22-54 kg) for males and 25 kg (range 20-34 kg) for females, which is 38% and 43% lower than expected for age and gender. Mean six-minute walk (6MW) was 465m for males and 499m for females, which is 22% and 4% lower than expected for age/gender/height/weight. In the 17 subjects with heart rate recovery (HRR) recorded after 6MW, the mean HRR at 1 minute (HRR1) was 20 bpm (range 0-46). 31% of tested subjects had a HRR1 consistent with impaired HRR (12 bpm or fewer). HRR negatively correlated with age (HRR1 B=-1.1; 95% CI -0.2 - -2; p<0.05). Half of the subjects had mild cognitive impairment (MoCA score < 26). MoCA scores correlated with literacy testing (B= 0.39; 95% CI 0.10-0.68; p=0.02).
The first 12 subjects wore the activity monitor 6 days (range 4-8 days) for an average of 15 hours a day. Average activity was sedentary for 7 hours (47%), light 7.5 hours (50%), and moderate 1 hour (7%) per day. There was a median of 7070 steps/day.
Conclusions
We found FGA to be feasible, acceptable, and safe. The duration of the FGA in our population was 3 times longer than the FGA for oncology. One of our most remarkable findings is that the older adults with SCD in this study have a physical function similar to non-SCD adults over the age of 80. They also demonstrate impaired HRR, an independent predictor of mortality in the elderly. After completion of the 12-month follow-up assessments, we will develop a briefer assessment to be evaluated in a larger study. Future steps will be to determine if FGA can predict outcomes such as risk of hospitalization and mortality and to develop interventions to improve these outcomes.
Strouse:Global Blood Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal