Multiple Myeloma (MM) remains a cancer of terminally-differentiated plasma cells that reside predominantly within the bone marrow. Malignant plasma cells are nurtured by a permissive microenvironment that favors tumor progression, drug resistance and disease relapse. Recurrent somatic mutations in hematopoietic stem cells, the source of major components in bone marrow niche, lead to age-associated clonal hematopoiesis of indetermined potential (CHIP) and has been associated with inferior survivals among individuals without malignant hematologic disorders. It is possible that these mutations in non-MM cells would affect remission time after transplant. We performed whole exome sequencing to identify CHIP-associated mutations within the autograft utilized to rescue hematopoiesis after high dose melphalan and autologous hematopoietic cell transplant (HCT). We then correlated the presence of CHIP with the outcome of MM patients (pts) following autologous HCT.
Methods. MM pts (N=101) that underwent HCT between 2006 and 2017 were studied. DNA was extracted from 1 ml of cryopreserved mobilized hematopoietic cell product. Targeted sequencing was then performed using Tempus xE whole exome platform (Tempus, Chicago, IL) with variable allele frequency (VAF) ≥0.1. Progression-free survival (PFS) and overall survival (OS) were defined as the time from transplantation until event of interest, with censoring at time of last follow up. Cox regression was used for time-to-event outcomes; hazard ratios (HR) and 95% confidence intervals (CI) were reported. P-values were two-sided and those <0.05 were considered statistically significant.
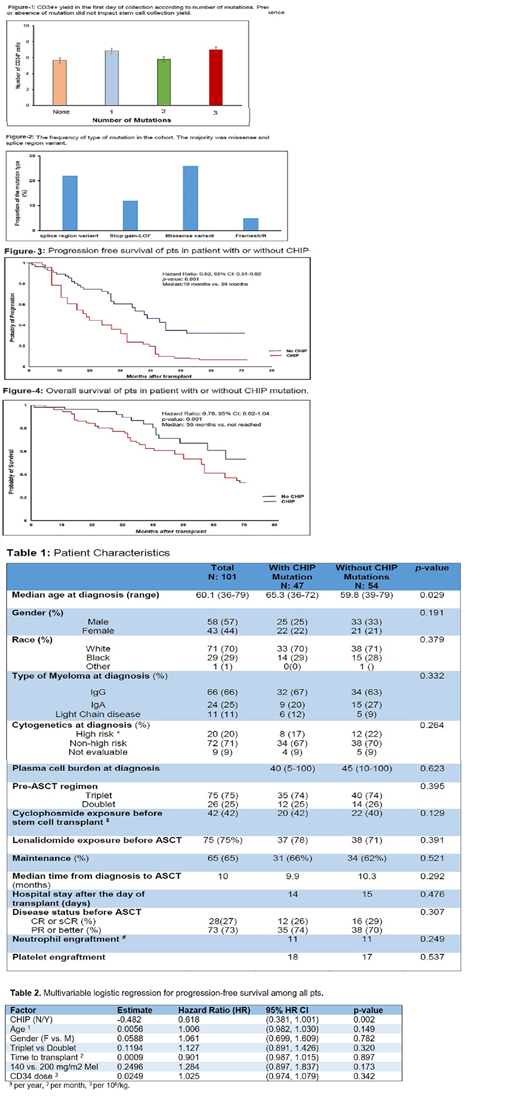
Results. The median age was 60.1 years at the time of HCT. 58 pts were male and 43 female; 29 pts were African-American, 1 Asian/Indian and 71 were Caucasian. Seventy five (75%) and 42 (43%) pts had prior exposure to lenalidomide or cyclophosphamide, respectively. Thirty two pts (32%) underwent hematopoietic cell mobilization with GCS-F and plerixafor, 38 pts (38%) with cyclophosphamide and 31 pts (31%) with GCS-F alone. Forty seven pts (47%) had at least one CHIP-associated mutation. The median number of CD34+ yield in the first day was 6.7 x 10e6/kg for pts with CHIP mutations and 5.64 x 10e6/kg for pts without any CHIP mutation (p = 0.4). The presence or absence of CHIP mutations did not impact the yield of CD34+ stem cells collected (Fig. 1).
The majority of mutations were either missense variants or mRNA splicing variations (Fig. 2), most commonly SF3B1, ASXL1, TET2 and ASXL2. CHIP mutations were associated with increased age (p= 0.021), but there was no association with prior history of previous cancer, smoking, cytogenetically-defined high risk disease, pre-HCT hemoglobin level or red blood cell mean corpuscular volume. There was also no significant difference between the transplant course between the two groups in terms of neutrophil and platelet engraftment or length of hospital stay.
Median follow up was 32 months. During follow up 3 pts develop MDS/AML (2 pts in the CHIP group and one in no CHIP group). Coronary artery disease was the cause of death in one patient in CHIP cohort versus none in the CHIP negative cohort. Myeloma progression was the major cause of death in CHIP and No CHIP cohorts (66% vs. 60%, p=0.48). Median PFS was 19 months in CHIP cohort vs. 39 months in No CHIP group (HR: 0.62, 95% CI: 0.51-0.92, p= 0.001). Median OS has not been reached in the No CHIP group while it was 56 months in CHIP group (HR: 0.78, 95% CI: 0.62-1.04, P=0.09). In multivariate analysis, presence of CHIP remained a significant predictor of worse PFS after adjusting for age, maintenance therapy, high risk disease, performance status, triplet vs. doublet pre-SCT therapy, melphalan dose and MM genetic risk. (Table 2).
Conclusion: Here we showed high frequency of large clonal hematopoiesis clones (i.e., VAF ≥0.1) in autograft of MM pts. The presence of this mutations does not impact stem cell yield or transplant course, however it impacts PFS independent of age and other unfavorable factors. Our data highlights high frequency of SF3B1; the role of this mutant in modulating apoptotic factors in myeloma microenvironment should be investigated.
Malek:Celgene: Consultancy; Amgen: Speakers Bureau; Adaptive: Consultancy; Janssen: Speakers Bureau; Medpacto: Research Funding; Sanofi: Consultancy; Takeda: Consultancy. Caimi:ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Fate Therapeutics: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Kite Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Caldwell:Tempus Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal