Background
Acute myeloid leukemia (AML) in older adults is a biologically and clinically distinct entity. These patients often have comorbidities, and their treatment must be chosen with caution. In AML patients over 60y old, cure rates are under 10% even after intensive chemotherapy (CT).
Aim
To compare the efficacy of different therapeutic approaches in elderly AML-pts treated in NRCH.
Methods
From 2002 till 2019, NRCH has conducted a prospective non-randomized study which included 80 AML-patients 60-81y (Me - 67y): 60-65 yy (n=53) and >65y (n=27); M/F - 35/45; de novo AML n=61 (76,25%), AML from MDS - n=13 (16,25%), «secondary» AML - n=6 (7,5%); cytogenetic risk: favorable n=1 (1,25%), intermediate n=49 (61,25%), poor n=30 (37,5%).
The patients were stratified to different treatment approaches according to age. Patients 60-70y (n=40) mostly received 1-2 induction cycles 7+3 (ARA-C 100 mg/m2 bid; Dauno - 45-60 mg/m2 ), then 2 consolidation cycles 7+3 (Dauno - 45 mg/m2) and 2 years maintenance (5+5 with 6-MP). Patients >70y (n=22) were usually treated with 1-2 induction and 2 consolidation cycles of low dose Ara-C (LDAC) (10 mg/m2 sc bid, 28-days) and 3 years maintenance with 21-28-days LDAC. In some cases, fit patients over the age of 70y have got 7+3 (n=5) and some younger with comorbidities - LDAC (n=13).
The analysis was done in May 2019. We evaluated treatment outcome according to age, cytogenetics and type of CT.
Results
The CR rate in the whole group of elderly AML-pts was 57,5% (46/80) with a median CR-duration - 10 mon (1-138 mon), early death - 16,25% (13/80) and resistance - 26,25% (21/80) with no major differences in the two age cohorts (<>70y).
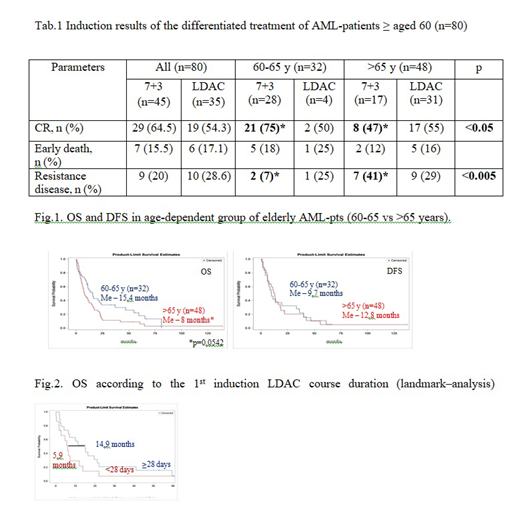
In order to assess of the efficacy of two chemotherapy options we have compared 7+3 and LDAC in patients aged 60-65 and older. In patients aged 60-65 CR-rate was higher -75% (21/28) after 7+3 vs 50% (2/4) after LDAC, with less resistant forms - 7% (2/28) vs 25% (1/4), respectively. In > 65y group CR-rate was identical in pts after 7+3 (47%, 8/17) and after LDAC (55%, 17/31) with similar numbers of resistant forms: 41% vs 29%. Early death rate did not differ among the groups. There was statistically higher CR-rate and lower resistant forms on 7+3 in pts aged 60-65 compared to older pts. - 75% vs 47% (p<0.05) and 7% vs 41% (<0.005) (Tab.1).
Long-term results in the whole cohort of elderly patients were as follows: 1-y OS - 46%, DFS - 52,2%, 5-y ОS - 13%, DFS - 9% with high relapse rate (70%) development, mostly with early occurrence (Me - 12.8 mon). The median survival was statistically longer in patients aged 60-65y (n=32) comparing to older ones (n=48) - 15.4 vs 8 mon, respectively (p=0.0542), but DFS was equal (Fig.1).
Higher incidence (87% vs 74%) and earlier relapse development (12 vs 16 mon) were registered in the group with poor cytogenetics comparing to favorable/intermediate (p=0,022). We didn't observe significant difference in long-term outcome of AML-pts older or younger 70y.
Standard LDAC duration is 10-14 days, twice less than we used in our study. A landmark-analysis (from day 30 of induction) has shown that, if the 1st course-duration was less than 28 days, the median survival was shorter - 5,9 mo in comparison with 14,9 mo in pts with 28-days LDAC (p=0.12). The efficacy of 28-days LDAC was very similar to 7+3, mainly in patients aged 66 and older (Fig.2).
Conclusion
The outcome in elderly AML-patients is determined by age (more or less 65y) and the group of cytogenetic prognosis (poor vs favorable/intermediate).
Intensive induction (7+3) is more preferable in patients aged 60-65 y as it produced the higher CR-rate and less resistant forms, results that are comparable to younger AML-patients. In patients older than 65y - CR-rate after 7+3 or 28-day LDAC was identical, and 28-days LDAC may become the choice of treatment for patients older than 65y. However long-term results are generally poor so new therapeutic strategies for elderly AML-patients are highly needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal