Comparative Analysis for Effectiveness of Azacitidine versus Decitabine in Acute Myeloid Leukemia and Myelodysplastic Syndromes with Marrow Fibrosis: A Single Institution Experience
Ala Ebaid, MD1, Shashank Cingam, MD1, Quiying Liu, MD2, Khine Z Win3, MD, Daniel Babu, MD4, Tawny Boyce, MS, MPH4, Cecilia Arana-Yi, MD1
Department of Internal Medicine, Hematology/Oncology, University of New Mexico, Albuquerque, NM.
Department of Internal Medicine, University of New Mexico, Albuquerque, NM.
University of California San Francisco.
University of New Mexico and Tricore Reference Laboratories
Department of Internal Medicine, Division of Epidemiology, Biostatistics and Preventive Medicine, University of New Mexico, Albuquerque, NM.
Introduction
The hypomethylating agents (HMA) azacitidine (AZA) and decitabine (DEC) are used clinically for the management of myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML); however, treatment responses and survival outcomes are very limited. Bone marrow fibrosis (MF) is present in 10-20% of MDS/AML and is predictor of poor responses to azacitidine and dismal survival outcomes. Genetic abnormalities including TP53 accumulation, WT1 gene expression, increased CXCL9 and CXCL10 among others contribute to the etiology of MF. The impact of MF in therapeutic responses and survival to AZA versus DEC has not been previously assessed.
Methods
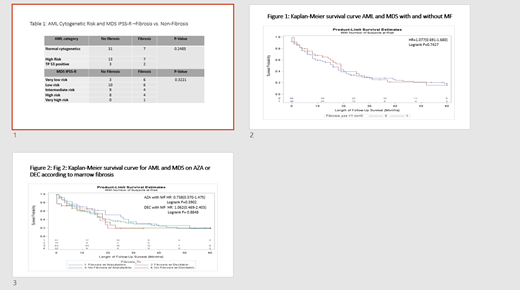
Retrospective chart review of cases from 2000-2019 at UNM Cancer Center to identify clinical characteristics, cytogenetic, molecular status, treatment and overall survival. AML patients were risk stratified according to ELN risk category, and MDS patients based on their IPSS-R scoring system. 142 bone marrow samples were analyzed for marrow fibrosis with hematoxylin and eosin-stained slides and confirmed with trichrome staining at Tricore Reference lab. 92 AML patients had a complete cytogenetics analysis.
The goal of this study is to evaluate the clinical, pathologic characteristics and survival outcomes of AML and MDS patients with and without MF treated with AZA compared to DEC at the University of New Mexico Comprehensive Cancer Center.
Results
142 patients with MDS (n=45, 31.7%) and AML (n=97, 68.3%) treated with AZA (n=85) 59.9%, and DEC (n=57) 40.1%. 45 patients have MF (31.7%) vs. 97 patients without MF (68.3%).
39.4% (n=56) were females, 31.7% had MDS (n=45), 68.3% had AML (n=97) and 31.7% (n=45) had MF.
The median age at diagnosis was 69.5 years for the AZA group and 68 years for the DEC group. In AML group there was 20 (20.8%) patients with high-risk cytogenetics and 38 (39.6%) with diploid cytogenetics. There was no statistical difference between the MF degree and the cytogenetics of the patients.
In the MDS group 9 patients (20%) with very low risk IPSS, 16 (35.6%) low risk, 13 (28.9%) intermediate and 13 (15.5%) patients with high and very high risk IPSS. In the fibrosis group 21 patients (46.7%) had low grade and 24 patients (53.3%) had high grade (MF2 and MF3). There were no significant differences in MF degree and IPSS or ELN categories.
Median duration of treatment was 3.2 months and median number of treatment cycles was 4 for AZA and 3 for DEC. There was no significant difference in median overall survival between two groups (AZA 18 months vs DEC 17 months, p=0.3355). Median overall survival was not significant in AZA group with de novo AML patients (AZA 19 months versus DEC 15 months, p=0.3013).
There were no OS differences in AML and MDS patients with MF. (Figure 1) Patients with MF on AZA had a trend toward better OS compared to DEC. (Figure 2) In MDS and AML, younger than 65 years old had better OS compared to older than 65 years. (p=0.011) In AML, TP53 mutation was associated with worsening survival outcomes. (median OS 2m vs 18m, p=0.0238)
Conclusions
The frequency of MF was 46.7% in MDS and 24.7 % of AML cases, higher than reported in other studies. However, MF did not affect survival outcomes of MDS/AML treated with AZA or DEC. Although non-statistically significant, MF cases had a trend towards better survival on AZA compared to DEC. The presence of TP53 was associated with decreased survival in AML patients with fibrosis.
Our study confirms that MF is a common feature in MDS/AML in New Mexico, but does not influence survival outcomes in patients treated with AZA or DEC.
Arana Yi:Jazz Pharmaceuticals: Other: Advisory Board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal