
Introduction: Venetoclax (VEN), a selective BCL-2 inhibitor, in combination with hypomethylating agents (HMA) has high efficacy in treatment-naïve elderly patients with acute myeloid leukemia (AML). The role for VEN in patients with relapsed/refractory (R/R) AML, myelodysplastic syndrome (MDS), or other myeloproliferative neoplasms remains incompletely defined. In particular, the efficacy of VEN+HMA has not been studied systematically in patients who experience AML relapse following allogeneic hematopoietic cell transplantation (HCT).
Method: All patients treated with VEN+HMA (azacitidine or decitabine) for R/R de novo or secondary AML or progressive MDS following allogeneic HCT were identified and reviewed retrospectively. All included AML patients had overt clinical relapse with ≥ 5% bone marrow blasts or extramedullary disease biopsy proven to be AML. Patients were included in this analysis if they received at least 14 days of VEN therapy.
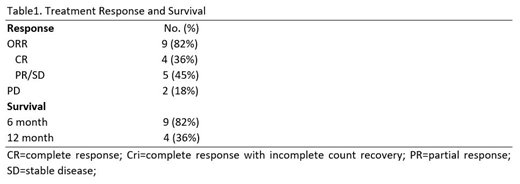
Results: Eleven patients with median age 66 (range 25-75) were treated for R/R AML post-allogeneic HCT. Transplant characteristics included use of reduced intensity conditioning in 10/11 (91%), matched sibling donors in 5/11 (45%), matched unrelated donors in 5/11 (45%), and cord blood in 1/11 patients. The median time from HCT to relapse/disease progression was 7 months (range 3-36). Two patients had extramedullary relapse only, and the remainder had marrow involvement. Eight patients (73%) received azacitidine and 3 (27%) received decitabine in combination with VEN. All but two patients (82%) had prior HMA exposure and most received VEN+HMA as initial post-transplant salvage therapy (64%). Only one patient received donor lymphocyte infusion in conjunction with VEN+HMA therapy, and none proceeded to a second allotransplant. Nine patients (82%) experienced an objective response, which included 4 CR/CRi (36%) and 5 PR/SD (45%). In patients with CR/CRi, three patients had adverse risk cytogenetics and one had a favorable risk profile at diagnosis consisting of normal cytogenetics with an isolated NPM1 mutation. All patients who failed to remit with VEN+HMA had intermediate- or high-risk genetic features. The median number of treatment cycles given was 3 (range 1-20). Median survival was 11 months and estimated 6-month and 12-month survival was 82% and 36%, respectively. Three patients remain alive with median 16.5 months follow-up (range 2.5-32).
Conclusion: Venetoclax in combination with HMA is a viable salvage option in patients with relapsed AML or progressive MDS after allogeneic HCT, including those with prior exposure to HMA. Although one patient in this cohort sustained long term complete remission, overall prognosis remains dismal in this high-risk patient population and improved treatment options for relapsed/refractory AML following alloHCT remain needed.
Damon:Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees. Martin:Amgen, Sanofi, Seattle Genetics: Research Funding; Roche and Juno: Consultancy. Olin:MedImmune: Research Funding; Ignyta: Research Funding; Clovis: Research Funding; AstraZeneca: Research Funding; Revolution Medicine: Consultancy; Daiichi Sankyo: Research Funding; Astellas: Research Funding; Genentech: Consultancy, Research Funding; Pfizer: Research Funding; Jazz Pharmaceuticals: Consultancy, Honoraria; Novartis: Research Funding; Mirati Therapeutics: Research Funding; Spectrum: Research Funding. Smith:Astellas Pharma: Research Funding; Abbvie: Research Funding; fujiFilm: Research Funding; Revolution Medicines: Research Funding. Logan:Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy; Pharmacyclics: Research Funding; Astellas: Research Funding; Jazz: Research Funding; Kite: Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees; TeneoBio: Consultancy; Kiadis: Consultancy; Kadmon: Research Funding; Abbvie: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal