INTRODUCTION
Appropriate restriction of blood transfusion is important to reduce harm to patients and cost to society. Current research shows that every RBC transfused unit increases 30-day mortality (odd ratio = 1.32), composite morbidity (odd ratio =1.23), pneumonia (odd ratio = 1.24) and sepsis/shock (odd ratio = 1.29) of 95% Confidence Interval. Literature shows that it is feasible to significantly reduce healthcare costs and potential transfusion-related harm by minimizing blood transfusion orders. This will help improve transfusion quality, minimize administrative cost, and maximize patient safety.
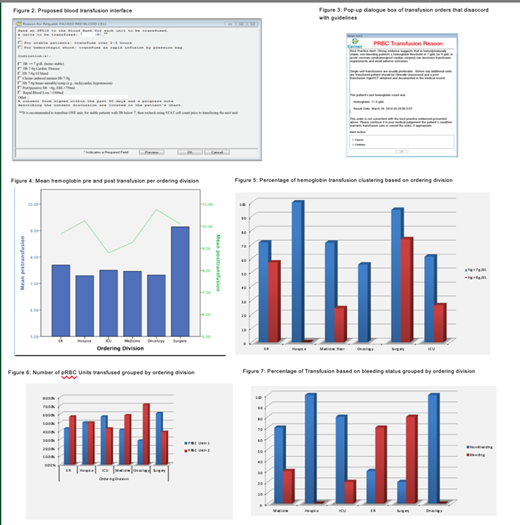
We examined the extent of adherence to the American Association of Blood Banks (AABB) transfusion guidelines by reviewing blood transfusions orders that were fulfilled throughout the year of 2018, and the potential effect of quality improvement intervention.
OBJECTIVES
The objective of this research is to restrict blood transfusion products through the implementation of an automated process that accords with current guidelines. The process entails modifying the current interface at the VA Palm Beach and effectively create an embedded clinical decision-making system that includes appropriate logistics to guide the appropriateness of blood transfusion orders. The interface promises interactive pop-up dialogue that engages users with a set of rules to assess transfusion indication and guide its appropriateness. The proposed intervention provides safer evidence-based transfusion, reduced risk of non-infectious adverse events and infectious agents, and decreased demand on limited blood supplies.
METHODS
This is a retrospective analysis of transfused patients in year 2018 .The data was retrieved from an electronic medical record database, which included patient gender, age, comorbidities, mean baseline hemoglobin, pre- and post- transfusion hemoglobin, hemodynamics status, complications, active bleeding, history of cardiac disease, ordering division, and number of units transfused.
Patients were randomly selected from January to August 2018 (n=204). Roughly 302 PRBC units were transfused, averaging 1.4 units per person. Insignificant life-threatening complications were reported. The Average pre-transfusion hemoglobin was 7.6, and post-transfusion hemoglobin was 9.3. 54% received 2 units, whereas 46% received 1 unit.
INTERVENTIONS
We propose a two-tier auditing system, based on a low and high priority, which reflects the timeline to address non-compliant transfusion orders. Low priority orders are evaluated during the periodic meeting of the transfusion committee, and high priority orders are addressed within a few hours of the transfusion order. All transfusion orders of Hg > 7-8 g/dL are flagged with low priority, whereas those with Hg> 8g/dl and/or with orders exceeding one unit are flagged with high priority.
The intervention includes: Identify the key Stakeholders and seek appropriate approvals, modify the existing interface to comply with AABB transfusion guidelines, establish a cultural change of blood management, "Every One (unit) Matters", educate our staff, physicians, residents, and students, through didactic channels on guidelines, and present case reports on patient safety.
RESULTS
The system was embedded with a logging mechanism to record non-compliant order requests, collect pre and post intervention data, audit transfusion records, restrict transfusions to 1 unit per order. Each unit is treated as a unique clinical decision, and each patient is evaluated for symptoms upon every transfusion. The interface also includes a logistics serving as a clinical decision tool and as an advisory delineating transfusion indication. Each transfusion order placed that doesn't meet requirements is reviewed retrospectively and is considered a fall out and flagged for chart review. Cases are escalated to the medical review committee, based on auditing priority, and the ordering physician is contacted accordingly.
CONCLUSION
Each unit blood transfused is associated with incrementally increased risk for adverse outcomes. Improvement of the overall transfusion rate is a key component to the success of this project. Our future directions are to engage and earn the confidence of all divisions, as well as change the existing culture in order to promote evidence-based medicine and safer practices in a cost-effective manner.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal