Introduction:
Pancreatic cancer (PC) has a known association with venous thromboembolism (VTE), with incidence of approximately 17%. There is limited published data about trends and outcomes of PC patients with VTE. The purpose of this study was to describe the prevalence and mortality trends in PC with VTE and analyze VTE impact on hospitalized PC patients from 1998 to 2016.
Methods:
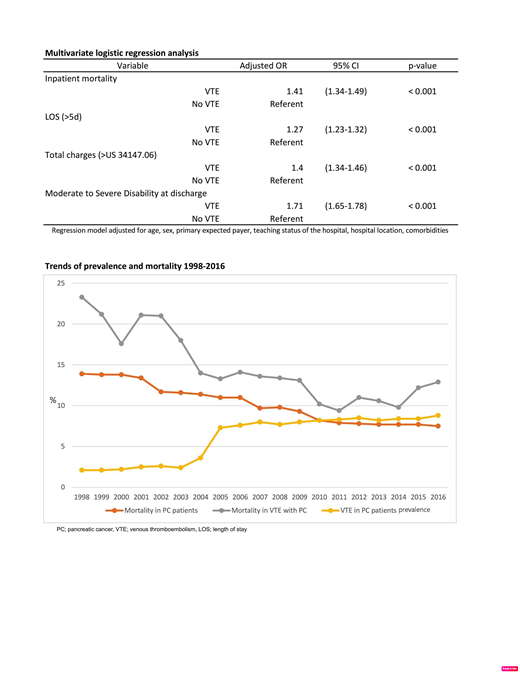
We analyzed data from the National Inpatient Sample (NIS) database of the Agency of Healthcare Research and Quality (AHRQ). Adults≥18 years with PC as well as presence of VTE were identified by using ICD-9 or ICD-10 codes. Cost of hospitalization was adjusted for inflation in reference to 2016. Comorbidities were classified using the Elixhauser comorbidity index. Demographic characteristics, trends and in-hospital outcomes between PC with and without VTE were compared. Multiple logistic regression was used to obtain risk-adjusted odds ratio (OR) to compare inpatient mortality, length of stay (LOS), total charges, and disability at discharge between PC patients with and without VTE. The regression model was adjusted for age, sex, primary expected payer, teaching status of the hospital, hospital location, and presence of comorbid conditions.
Results:
96,777 (6.5%) of a total of 1,488,543 hospitalized PC patients had an accompanying diagnosis of VTE. Mean age of the study population was 67 years. African Americans, younger age, and metastatic disease are associated with higher VTE prevalence rate. After adjusting for potential confounders, compared with those without VTE, PC patients with VTE had significantly higher inpatient mortality (12.6% vs 9.7%; OR, 1.41 [confidence interval (CI), 1.34-1.49]; P<0.001), longer LOS (8.04 vs 7.98 days; OR, 1.27 [CI, 1.23-1.32]; P<0.001), higher average cost of hospitalization (US $71,332 vs US $57,117; OR, 1.4 [CI, 1.34-1.46]; P<0.001), and greater likelihood of moderate to severe disability (defined as any beyond routine home discharge; ranging from short-term stay to skilled nursing facility to death upon discharge) (62.2% vs 50.6%, OR, 1.71 [CI, 1.65-1.78]; P<0.001). Although the annual prevalence of VTE among PC increased from 2.1% to 8.8%, in-hospital mortality declined from 23.3% in 1998 to 12.9% in 2016 (P<0.001).
Conclusion:
In the NIS cohort of hospitalized patients with PC and VTE from 1998-2016, annual prevalence increased while mortality overall decreased. When compared to patients without VTE, PC patients with VTE had higher inpatient mortality, longer length of stay, higher hospital cost and higher degree of disability upon discharge. Consideration for anticoagulation and interventions to limit VTE in PC patients may improve in-hospital outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal