INTRODUCTION: The prevalence of thrombotic complications in lymphoma patients ranges from 1.5% up to 59.5%. Lymphoma patients have a 10-fold higher risk for the development of venous thrombosis than patients with lung and gastrointestinal cancers. The pathogenesis of thromboembolic disease in hematological malignancies is complex and multifactorial and can be due to the underlying disorder or related to therapy. A number of biomarkers are associated with the occurence of VTE in cancer patients. Biomarkers reflect activation of coagulation and increased inflammatory potential. This study aimed to profile hemostatic and inflammatory biomarkers in patients with Hodgkin lymphoma, non-Hodgkin lymphoma, and chronic lymphocytic leukemia/ small lymphocytic lymphoma.
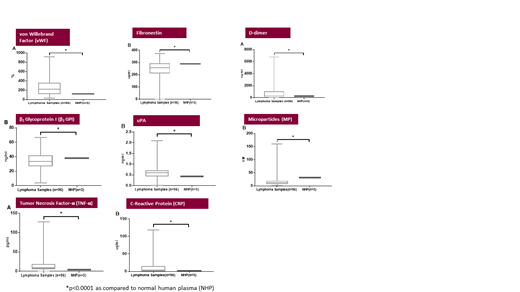
METHODS: Citrated plasma samples were collected from lymphoma patients (n=96) under an IRB approved protocol Clinic for hematology, Lymphoma Center, University of Belgrade in Serbia. Samples were shipped to Loyola University Chicago and analyzed in batches via commercially available ELISA kits to profile biomarkers of coagulation activation and inflammation. Markers in Coagulation Activation: von Willebrand Factor (vWF), Factor XIIIa, Protein S, β2Glycoprotein I (β2GPI), D-dimer, Microparticles (MP), Urokinase-type Plasminogen Activator Antigen (uPA), Fibronectin. Markers of Inflammation included: Human Tumor Necrosis Factor- α (TNF- α), C-Reactive Protein (CRP), Plasminogen Activator Inhibitor Type 1 (PAI-1). The lymphoma patient population for each biomarker was compared to normal human pooled plasma (repeated 3 times for each biomarker), which consisted of 25 male and 25 females.
RESULTS: The mean patients' age was 56 years (range, 19-80 years); 52.4% were males. Most patients were newly diagnosed and had advanced stage disease. A total of 42 patients (43.8%) had high-grade NHL; 17 (17.7%) had low-grade NHL; 24 (25.0%) had HLL; 7(7.3%) had HL; 6 (6.3%) had other forms. Lymphoma patients had significantly dysregulated following markers of coagulation: vWF, β2GPI, D-dimer, MP, uPA, and Fibronectin (Figure 1) (p<0.001 for all in comparison to controls). TNF-α and CRP as markers of inflammation were also significantly increased in lymphoma patients (Figure 1) (p<0.001 for both in comparison to controls). In lymphoma population 12 patients had thrombosis. Patients with thrombosis had significantly higher Factor XIIIa in comparison to lymphoma patients without thrombosis (106±9 vs. 85±256; p<0.001).
CONCLUSION: Hemostatic dysregulation and inflammation is present in lymphoma patients, which may reflect increased thrombogenic potential. Further studies are required to link clinical data and biomarker levels, with special emphasis on the involvement of FXIII in the development of thrombotic events in lymphoma patients. Biomarker profiling of lymphoma patients will also help in the understanding of the pathophysiologic mechanisms involved in the observed thrombotic complications and differentiating the sub-groups.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal