Immune thrombocytopenia (ITP) is an autoimmune disease characterized by thrombocytopenia and increased risk of bleeding resulting from platelet destruction and impaired production. Treatment is indicated when there is active bleeding or there is an increased risk of bleeding. Many first- and second-line treatments exist but response to treatment is variable. Spontaneous remission of ITP has been reported in some patients, particularly those with earlier stage disease. Remission has also been reported with various ITP therapies e.g. corticosteroids, rituximab, thrombopoietin receptor agonists and splenectomy.
Fostamatinib is an oral spleen tyrosine kinase (Syk) inhibitor, recently approved for the treatment of chronic ITP in patients without adequate response to a prior line of therapy. It acts through inhibition of the platelet phagocytosis by the macrophages. In the two phase 3 trials, FIT 1 and 2, an overall response (≥50X109/L)occurred in in 43% of patients (Bussel et al. Am J Hematol. 2018; 93: 921-930). FIT involved two parallel, phase 3, randomized, double-blind, placebo-controlled trials where patients with persistent/chronic ITP were randomized 2:1 to fostamatinib or placebo. Responders and non-responders could enter an open-label phase at week 24.
We report here a patient who achieved prolonged treatment free response after a short course of fostamatinib.
A 66-year-old male, with previous medical history of coronary heart disease, presented with isolated thrombocytopenia (platelet count (PC) 56X109/L) in March 2015. The patient was on clopidogrel and acetyl salicylic acid that were initiated 6 months previously (PC at time of antiplatelet initiation: 147X109/L). Both medications were discontinued; nevertheless, PC continued to drop reaching 17X109/L. Clinically the patient had no signs of bleeding.
Diagnostic work up revealed thrombocytopenia on peripheral blood smear; increased number of megakaryocytes in bone marrow aspirate; and normal cytogenetics.
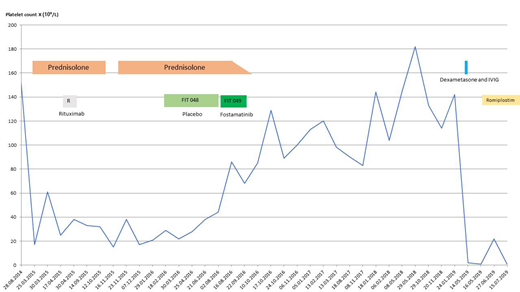
We started treatment with prednisolone 80 mg daily in March 2015. He continued at that dose for 4 weeks but with only minor effect on PC (maximum 25X109/L). We started gradual tapering of prednisolone dose until discontinuation. Because of the indication for antiplatelet therapy and persistently low PC, rituximab was administered and the patients received 4 weekly infusion. Treatment with rituximab resulted in an initial though transient increase in PC (figure); therefore prednisolone was re-initiated.
Following that the patients was included in FIT-48 study in February 2016 and was randomized to Placebo (PC at inclusion: 22X109/L) (figure). Study medication dosage was escalated according to the study protocol. The patient was on a stable prednisolone dose of 12.5 mg daily upon entry. He experienced no side effects. He continued on study medication for 24 weeks (PC at the end of study: 44X109/L). The patient entered the open-label study (FIT049-study) in August 2016 and received fostamatinib 100mgX2. PC increased within 2 weeks after initiation of fostamatinib to 86X109/L and we began tapering prednisone dose down to 5 mg over 2 months. During this time his PC ranged between 54-86X109/L. Unfortunately, the patient developed moderate diarrhea, which led to the discontinuation of fostamatinib after 7 weeks (PC 85X109/L). Diarrhea resolved after discontinuation.
During the next 2.5 years, PC ranged between 80-140X109/L without any treatment. In May 2019, he presented with PC 5X109/L and muco-cutaneous bleeding indicating relapse. The patient did not respond to corticosteroids and IVIG, but responded to a maximum dose of romiplostim (platelet count 20X109/L).
Our patient failed several ITP therapies during the course of disease but seemed to have responded to fostamatinib. The patient did not tolerate fostamatinib and had to discontinue the medication because of diarrhea - a known side effect of fostamatinib. However, the platelet count did not fall after fostamatinib discontinuation and the patient remained in response which lasted for 2.5 years. To our knowledge this is the first case report of long-lasting treatment free response following a short treatment course of fostamatinib.
Ghanima:Amgen: Consultancy, Honoraria; Bayer: Honoraria, Research Funding; Pfizer/BMS: Research Funding; Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal