Introduction Langerhans cell histiocytosis (LCH) is a rare disease involving clonal proliferation of Langerhans cells. The reported incidence of LCH ranges from 0.5-5.4 cases per million persons per year, according to the prospective registry-based reports. However, due to the rarity of the disease and the limitation of prospective registries, the comprehensive understanding of nation-wide epidemiology has been limited. This study aimed to analyze the incidence by age and diagnostic patterns of LCH using the population-wide healthcare database in Korea.
Methods The claims data of the Health Insurance Review and Assessment (HIRA) contain information of 46 million patients per year, which accounts for about 95% of the total population of South Korea. The data include information regarding diagnoses, hospitalization, and prescription drugs. Since 2005, the "National cancer registration and reimbursement program" has been implemented, which reimburse for 90% of the medical expenses of patients with malignant diseases, including LCH. Therefore, all the patients with LCH have been registered in the database after a definite diagnosis. From the HIRA open data source, we extracted a claim data of patients corresponding to diagnosis codes of C95.0 (Multifocal and multisystemic -disseminated LCH), C96.5 (Multifocal and unisystemic LCH), or C96.6 (Unifocal LCH) during the period of 2010-2017. Data for 2010-2011 was used as a reference for overlapping patients, and the actual analysis was conducted with data from 2012 to 2017.
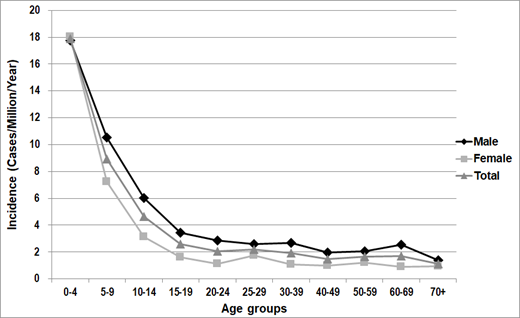
Results During the period, a total of 59,929 insurance statements were issued, and 53,446 statements with only one identical diagnostic code and confirmative workups were selected for final analysis. The total incidence cases during the period of 2012 to 2017 were 899 cases, and the average number of the annual incidence was 150 cases. The incidence was 3.0 cases per million persons per year. There was a male predominance with a male-to-female ratio of 1.63:1 (558 cases:341 cases) in a whole cohort. For the detailed diagnosis codes, C96.6 was the most frequent as 93.4%, followed by C96.0 as 4.9%, and C96.5 as 1.7%. The average age at diagnosis was 26.6 years (range, 0.2~87 years) in all incidence cases, and 26.6 years for C96.0 group, 29.5 years for C96.5 group, and 25.9 years for C96.6 group, respectively. When patients were grouped by age at diagnosis, the age group of 0-4 years showed the highest annual incidence of 17.9 cases per million, followed by the group of 5-9 years as 8.9 cases per million, and the age group over 70 years showed the lowest annual incidence of 1.1 cases per million (Figure 1). There were no seasonal trends in the diagnosis of LCH. At diagnosis, 21.6% of patients were diagnosed at the department of neurosurgery, 21.5% at pediatrics, 19.3% at internal medicine, and 16.8% at orthopedic surgery. For examinations conducted at the time of diagnosis, simple radiography was conducted in 84.9% of patients, computed tomography in 32%, magnetic resonance imaging in 39.6%, bone scan in 47.1%, and bone marrow examination in 22.9% of patients. For treatment, most of the patients (93.7%) received at least one modality of treatments after diagnosis; 42.7% of patients underwent surgery only, 30.4% received topical steroids only, 12.6% underwent surgery followed by chemotherapy, and 10.5% received chemotherapy. For chemotherapy, vinblastine was the most frequently prescribed drug as used in 82.9% of patients who received chemotherapy, followed by methotrexate in 39.4%, and mercaptopurine in 38.9%.
Conclusions This study was the first big data analysis regarding LCH in Korea, and the annual incidence of LCH was 3.0 cases per million persons per year. The incidence was highest at 0-4 years of age, and the incidence was significantly decreased with age. We plan to conduct further research on the treatment and outcomes of Korean LCH patients in conjunction with the data of ongoing prospective registry.
Figure 1. The annual incidence of Langerhans Cell Histiocytosis by age at diagnosis
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal