Introduction: Sickle cell disease (SCD) is one of the most common inherited hematological disorder in the United States. Sickle cell crisis is a common complication caused by excessive sickling of red blood cells, resulting in tissue ischemia. The frequency of such pain crisis, however, varies greatly among patients depending on disease control and other patient characteristics. Asthma is a common comorbidity in SCD patients which is associated with higher incidence of acute chest syndrome (ACS). However, the impact of asthma on short term outcome of acute sickle cell crisis remains unclear.
Methods: We analyzed data from the National Inpatient Sample database. Data entries from year 2005 through 2014 were included. The presence of SCD, sickle cell crisis, ACS, asthma are identified using corresponding ICD codes. Data regarding demographic information, performed procedures, inpatient mortality, and length of stay are extracted and analyzed accordingly.
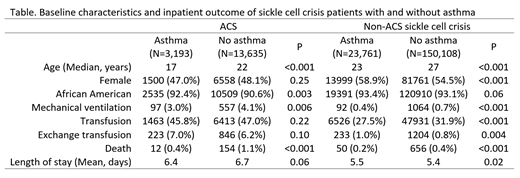
Results: A total of 247,266 records were identified. The median age at admission was 26 years (interquartile range 18 - 37), with most patients being of African American origin (91.8%). A total of 16,828 (6.8%) patients presented with ACS, whereas 173,869 (70.3%) presented with non-ACS crisis. The remaining 56,569 (22.9%) patients were admitted for reasons other than sickle cell crisis, most commonly infection. Overall, 34,609 patients (14.0%) had asthma. Compared to patients without ACS, the incidence of asthma was significantly higher in patients with ACS (19.0% vs 13.6%, P<0.001), whereas patients with non-ACS crisis had a similar incidence of asthma compared to those without sickle cell crisis (13.7% vs 13.5%, P=0.42). Asthma patients who presented with ACS exhibited a lower inpatient mortality (0.4% vs 1.1%, P<0.001), as well as lower use of invasive mechanical ventilation (3.0% vs 4.1%, P=0.006). Similarly, in patients with non-ACS sickle cell crisis, asthma was associated with lower mortality (0.4% vs 0.2%, P<0.001), lower use of invasive mechanical ventilation (0.4% vs 0.7%, P<0.001), and lower frequency of transfusion (27.5% vs 31.9%, P<0.001).
Conclusion: Our study again demonstrated the association between asthma and ACS in SCD patients. Furthermore, asthma appears to be associated with superior outcome in both patients with ACS and non-ACS sickle cell crisis. Further studies are warranted to elucidate if asthma is associated with a milder form of sickle cell crisis which may correlate with the physiologic basis of these associations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal