Background;
Transfusion-dependent β-thalassemia (TDT) is a severe form of congenital anemia. Regular blood transfusion and continual administration of iron-chelators are conventional therapeutic strategies in TDT. Despite progressive advancements in developing various iron scavenging drugs, iron overload is still considered a challenging conundrum in these patients. Multiple organ dysfunctions result from the toxic effect of excess iron deposition in parenchymal tissues that cause high morbidity and mortality among TDT patients. The greatest affected tissues include endocrine glands, liver, heart, and kidneys.
Aim of the study: To investigate pulmonary function of patients with TDT in relation to their iron overload.
Patients and Methods:
Pulmonary function tests were done for 10 Patient with TDT (table 1) in a well-equipped lung function unit in a tertiary care hospital by experienced respiratory technicians. An ideal test session was taken up following ATS/ERS recommendations. A proper grading system including acceptability and repeatability criteria was applied. Measurement of DLCO is done with a technique of single breath carbon monoxide (CO) uptake in the lung and lung volume is measured with gas dilution and body plethysmography. Chest x ray (CXR) was obtained in all patients.
Pulmonary function test was classified according to the following categories based on ATS/ERS criteria and American medical association criteria (AMA);
Normal: FEV1/FVC more than 70% FEV1, FVC, TLC, RV and DLCO normal (at least 80% predicted)
Obstructive: FEV1/FVC less than 70% FEV1 and FVC (less than 80% predicted). TLC and RV either normal or elevated (at least 120% predicted). DLCO normal (at least 80% predicted)
Restrictive: FEV1/FVC ratio (more than 70%) (1) FEV1, FVC, and TLC decreased (no more than 80% predicted) and a decrease in DLCO (no more than 80% predicted) or (2) TLC and RV decreased (no more than 80% predicted) with normal DLCO, FEV1, FVC, and FEV1/FVC, suggestive of low lung volumes, or (3) reduced TLC and DLCO.
Mixed obstructive and restrictive: FEV1/FVC ratio reduced, suggestive of obstructive disease. TLC and RV reduced, suggestive of restrictive disease. DLCO normal
Isolated low DLCO: DLCO decreased with normal FEV1, FVC, FEV1/FVC, TLC, and RV (As per AMA DLCO less than 75% were considered abnormal)
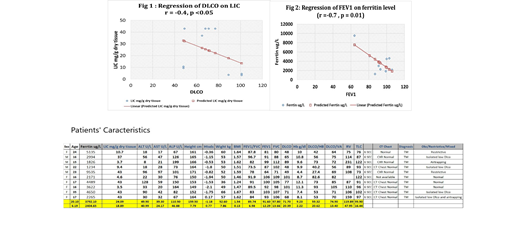
Results: In our 10 TDT patients 9 had normal CXR. One patient had minimal patchy ground glass opacity. Six patients (60%) had abnormally low DLCO indicating some impairment at the level of alveolar capillary membrane. None of them had obstructive pattern. However 2 patients had some air trapping. DLCO, DLCO/Hb, DLCO/VA and RV were correlated negatively with LIC (fig 1) . PFTs (DLCO, RV, and TLC) were correlated negatively with the LIC. In addition, FEV1 and FVC were correlated negatively with ferritin level (r = -0.7 and -0.77 respectively, p <0.01) (fig2).
Discussion: we documented a significant alveolar capillary membrane dysfunction in a good number of asymptomatic patients with TDT. This dysfunction appears to increase with advance of age. Iron deposition in the lung parenchyma appears to be the etiology of this abnormality as supported by the significant negative correlations between PFT parameters on the one hand and LIC and ferritin level on the other hand.
Conclusions:
Substantial alveolar capillary membrane dysfunction occurs in a good number of asymptomatic patients with TDT which is correlated with the degree of iron overload. Further studies are required to confirm these abnormalities on a large scale.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal