
Background:
Heart failure (HF) is a chronic medical condition that affects approximately 1-2% of the world's population and greater than 10% of those age 65 and older. Among patients with HF, iron deficiency (ID), defined as ferritin <100 ng/ml or transferrin saturation (TSat) <20% with ferritin 100-300 ng/ml, has an estimated prevalence of 30-50%, often without concomitant anemia. Thus, ID in HF is often underdiagnosed unless actively sought after. ID in HF has been shown to be an independent contributor of increased mortality, hospitalization and early readmission compared to HF patients without ID or HF patients with anemia without ID. A large trial, namely IRONOUT, illustrated the superiority of intravenous iron (IVFe) over oral iron supplements for HF patients who were identified as iron deficient. The FAIR-HF and CONFIRM-HF trials showed improved functional outcomes and quality of life in HF patients treated with IVFe and that these benefits were conferred even 1 year after treatment. However, these trials focus on iron store correction in patients with chronic heart failure patients. Little data are available regarding the correction of ID in patients who are admitted to hospitals for HF exacerbations.
Methods:
We performed a retrospective analysis of hospital records of patients admitted with HF as a primary or secondary diagnosis to a city-based large academic teaching health system between April 1, 2014 and April 1, 2017. Thereafter, we identified those patients who had sufficient iron studies (hemoglobin, iron, ferritin, transferrin, TSat) during their hospitalization to diagnose ID, as per the criteria above. Patients with ID were then stratified into those that did and did not receive IVFe. Patient charts were evaluated to two primary endpoints, namely one-year readmissions for HF and patient mortality.
Results:
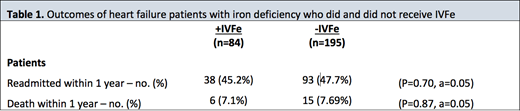
In total, 390 patients had sufficient iron studies performed to assess ID status, of which 279 met criteria for ID (71.5%). Eighty-four of the 279 patients received IVFe. Amongst patients that received IVFe, 38 patients were readmitted for HF (45.2%) and 6 patient deaths occurred within 1 year (7.14%). Amongst the remaining 195 patients who did not receive IVFe, 93 were readmitted for HF (47.69%) and 15 patient deaths occurred within 1 year (7.69%).
Conclusion:
These data suggest that despite clinical benefit in patient functional outcomes and overall quality of life in chronic heart failure patients treated with IVFe, treatment of ID in acute HF patients does not result in a reduction in admissions for HF or improvements in patient mortality.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal