Significance
Patients with acute myeloid leukemia (AML) are at high risk of critical illness requiring admission to the intensive care unit (ICU) due to both disease- and treatment-related complications. A better understanding of risk factors for ICU admission and prognosis may help with prevention of life-threatening complications and informed decision-making when treating AML patients.
Methods
This study included all adult Danish AML patients, who received remission-induction chemotherapy alone or in combination with allogeneic stem cell transplantation from 2005 to 2016. The cohort was identified using the Danish Acute Leukemia Registry (DNLR) and information on ICU admission was obtained from the Danish Intensive Care Database. We examined risk of ICU admission within 1 and 3 years of diagnosis considering competing risk of death and investigated a number of possible risk factors for ICU admission. We computed 1-, 3-, and 5-year mortality from time of ICU admission and in the matched non-ICU comparison group using a risk set matching (1:1) on time since diagnosis, sex, and age. Finally, we used the pseudo-value approach to compute the relative risk (RR) of death in the ICU admitted cohort compared to the matched cohort. We adjusted for ECOG/WHO performance status (PS), year of diagnosis, cytogenetic risk group, number of comorbidities, and secondary/therapy-related AML.
Results
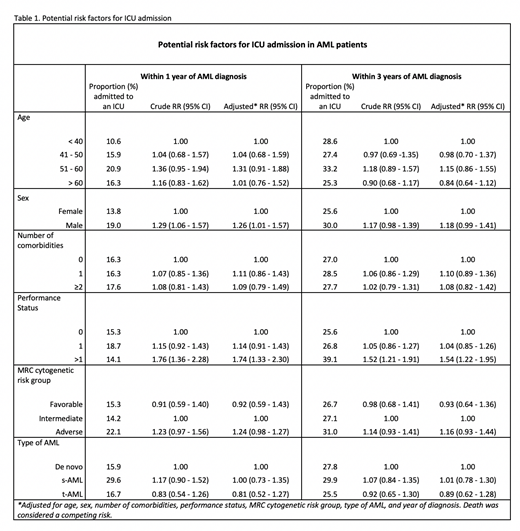
A total of 1383 AML patients were included in the study. The median follow-up time was 1.65 (IQR: 0.60-4.36) years. The risk of ICU admission within 1 year of AML diagnosis was 22.7%, and the risk within 3 years was 28.1%. Median time to ICU was 59 (IQR: 15-272) days. Male sex was associated with increased risk of ICU admission after 1 year (adjusted RR: 1.26, 95% CI: 1.01-1.57) and PS >1 was associated with an increased risk after both 1 year (adjusted RR: 1.74, 95% CI: 1.33-1.30) and 3 years (adjusted RR: 1.54, 95% CI: 1.22-1.96). Other factors listed in Table 1 (age, comorbidity, cytogenetic risk group, secondary or therapy-related AML, and year of diagnosis) were not associated with increased risk of ICU admission.
In AML patients admitted to the ICU, the 1-year mortality from time of ICU admission was 69.2%, compared to a 1-year mortality rate of 31.0% in the matched non-ICU patients (adjusted RR: 3.25, 95% CI: 2.56-4.12). Long-term mortality was increased in ICU patients; 3-year mortality was 82.1% compared to 49.7% (adjusted RR: 2.43, 95% CI: 1.97-3.01), and the 5-year mortality was 83.1% compared to 60.6%, (adjusted RR: 2.12, 95% CI: 1.70-2.66).
Conclusion
In this national population-based cohort study, more than one fourth of AML patients treated with remission-induction chemotherapy were admitted to an ICU within 3 years of diagnosis with the majority of ICU admissions occurring within the first year. ICU admission was associated with high mortality, especially within the first year after admission. The risk of mortality decreased over time but remained increased 3 and 5 years after admission compared to the matched cohort. Early monitoring and management of high-risk patients may be effective in preventing ICU admissions and PS may serve as a possible tool to identify patients at high risk of ICU admission.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal