Background
As with other complex therapies, treatment of AML varies among centers (ctrs) due to differences in patients (pts), infrastructure and care delivery models. Variation in ctrs practices, experience and resources may influence pt outcomes. Few studies have examined the association of ctr characteristics and survival in AML. Previous research offers conflicting results regarding outcomes of AML pts treated in National Cancer Institute Comprehensive Cancer Centers (NCICCC) versus community settings; neither study investigated ctr-level differences other than volume. We sought to compare AML outcomes in any of the HCA Healthcare (HCA) network of 131 community hospitals from 2011-18 with those reported in the Surveillance, Epidemiology, and End Results (SEER) database. We then examined pt, disease and center-related characteristics influencing outcomes in HCA hospitals.
Methods
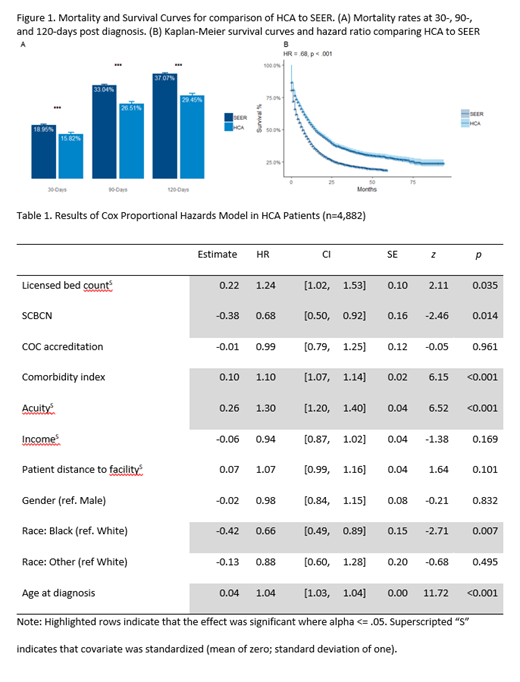
We identified pts with AML (excluding APL) > 18 yrs treated between 10/31/11 and 10/31/18 in an HCA hospital (N = 4,882) and obtained pt level data from electronic medical records. A comparative population treated was developed from the most recent SEER database (2011-15; N = 19,349). We used coarsened exact matching to control for as many potential biases as possible. We compared mortality at 30, 90 and 120-days and overall survival curves between HCA and SEER . A Cox regression model was used to investigate differences in hazard rates among HCA facilities while simultaneously assessing the impact of patient characteristics and facility characteristics. Of the HCA patients, 1339 were treated in 6 hospitals that meet defined metrics of infrastructure, staffing, processes and volume as part of certification to participate in the Sarah Cannon Blood Cancer Network (SCBCN).
Results
Matching for age, gender and race, HCA pts were found to have significantly lower mortality than SEER at 30, 90 and 120 days (p<.001) as well as significantly better survival (p<0.001; fig.1). We next investigated how pt and facility characteristics interact to predict outcomes for HCA patients (table 1). Elevated White Count at diagnosis (HR=1.3), Charlson index (HR=1.1), older age (HR= 1.04), and receiving treatment at a hospital with larger bed count (HR=1.26) were associated with significantly worse survival. Commission on Cancer (COC) accreditation status, Socio-economic status (SES), distance to facility, and gender did not significantly impact risk. Being treated in the SCBCN (HR=0.68) and African American race (HR= 0.66) were associated with improved survival
Conclusions
Previous research utilizing registry data demonstrated better survival for pts with AML treated in higher volume centers but provides conflicting information about survival for pts treated in a NCICCC versus a community setting. Neither study examined center characteristics beyond NCI designation. This report examines a large pt cohort treated in community hospitals across the US. Pts treated in these hospitals had significantly better survival than a matched cohort from the SEER database. We validate the importance of age, acuity and Charlson index as adverse factors. Analysis of facility characteristics demonstrated that qualification as a member of SCBCN was associated with improved survival underscoring the importance of infrastructure, quality systems and volume in achieving improved outcomes.
Lemaistre:HCA: Employment. Chao:HCA: Employment. Cruz:1. Daiichi Sankyo advisory board: Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Speakers Bureau. Eghtedar:Verastem Oncology: Consultancy; Novartis: Consultancy, Honoraria, Speakers Bureau; Jazz: Consultancy, Honoraria, Speakers Bureau; Celgene: Honoraria, Speakers Bureau; Takeda: Honoraria, Speakers Bureau. Holder:Sarah Cannon: Employment. Malik:Kite Pharma: Honoraria. Rotta:Kadmon Corporation, LLC: Consultancy; Jazz: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal