Background: Patients (pts) diagnosed with non-Hodgkin lymphoma (NHL) have increased risk of venous thromboembolic event (VTE). Retrospective studies have observed the risk of VTE is not the same across lymphoma subtypes, with aggressive subtypes having higher risk than indolent lymphomas. Current VTE prediction models such as the Khorana score (K-Score) consider all lymphomas as having equal risk of VTE. We conducted retrospective time - based analyses to develop a VTE prediction model that includes lymphoma subtype as a risk factor.
Methods: We accessed the Hematologic Malignancies Database at University Hospitals Seidman Cancer Center and collected records of pts diagnosed with diffuse large B cell lymphoma (DLBCL) or follicular lymphoma (FL) between 2000 and 2016. Pts with CNS involvement or active anticoagulation were excluded. FL grade 3B pts were included in the DLBCL cohort. Information retrieved included demographic characteristics, baseline disease and laboratory parameters, as well as comorbidities and diagnosis of VTE, including radiographic confirmation. Time to VTE was measured from the date of NHL diagnosis to the date of VTE incidence or censored at the date of last follow-up for those without VTE. Cumulative incidence of VTE was estimated using Kaplan-Meier method and its difference among groups was examined by log-rank test. Cumulative incidence of VTE was also calculated considering death as competing risk and comparisons done using the Gray test. Cox proportional hazards model was used to evaluate the effect of continuous and categorical covariates on cumulative incidence of VTE and to identify prognostic factors of VTE. Fifty percent of the study participants were randomly assigned to training cohort or reserved as an independent validation cohort. Performance of multivariate models was evaluated using the Akaike Information Criterion (AIC) and Concordance Index (C-Index). The final models built using the training dataset were further validated using the validation cohort. All tests are two-sided and p-values ≤ 0.05 were considered statistically significant.
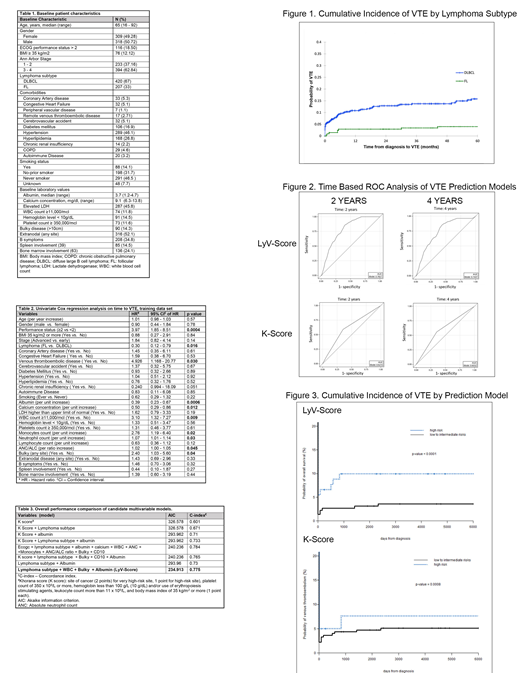
Results: We identified 627 pts with DLBCL (n=421) or FL (n=206) with available baseline characteristics, (Table 1). After a median follow up of 48 months (range 1-191), 77 pts experienced a VTE after NHL diagnosis. The cumulative incidence of VTE at 4 years for the whole cohort was 10.5% (95% CI 8.3-13.2). DLBCL pts had a significantly higher 4 - year cumulative incidence of VTE: 13.7% (95% CI 10.8-17.5) vs. 4.0% (95% CI 2.0 - 7.9) in FL pts (p <0.0001)(Figure 1).
Univariate analysis on the training cohort showed that lymphoma subtype (DLBCL vs. FL) was associated with incidence of VTE (p = 0.02); other baseline variables associated with VTE include ECOG performance status, bulky disease, history of VTE, and serum albumin, calcium, WBC count and WBC subtypes (Table 2).
Analysis of overall performance of multivariate models, including the K-Score as well as the variables identified in univariate analysis, demonstrated that the addition of lymphoma subtype and albumin to the K-Score improved the C-Index and the AIC (Table 3). The Lymphoma-specific VTE Score (LyV-Score) including lymphoma subtype, presence of bulky disease, baseline WBC and serum albumin resulted in improved performance, with C-Index of 0.775 and AIC of 234.913.
To further evaluate the performance of the LyV-Score model, we performed time - dependent ROC and calibration analyses. When applied to the training cohort, 2 and 4-year AUC for the LyV-Score were 0.7767 and 0.7463, respectively, whereas for the K-Score 2 and 4-year AUC were 0.6215 and 0.6032 (Figure 2). Time - based ROC analyses in the validation cohort confirmed the higher AUC achieved by the LyV-Score.
Cumulative incidence analyses show the LyV-Score and the K-Score identified groups with statistically significant differences in VTE risk (Figure 3), these differences were more marked between groups identified by the LyV-Score.
Conclusions: VTE risk models have considered all lymphoma subtypes as risk factor for VTE. We show this risk is not equivalent for all lymphoma subjects, with aggressive lymphoma patients presenting higher VTE risk. We have developed the LyV-Score as a VTE prediction model that incorporates NHL histologic subtype. This model shows improved performance over historic VTE risk models and can help identify lymphoma patients that may benefit from interventions to prevent VTE.
Malek:Celgene: Consultancy; Takeda: Consultancy; Sanofi: Consultancy; Medpacto: Research Funding; Janssen: Speakers Bureau; Amgen: Speakers Bureau; Adaptive: Consultancy. Metheny:Takeda: Speakers Bureau; Incyte: Speakers Bureau. Caimi:Genentech: Research Funding; ADC Therapeutics: Research Funding; Celgene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal