Introduction: Early readmissions are important indicators of quality of health-care. National-level data is currently lacking for patients admitted for induction chemotherapy for acute myeloid leukemia (AML). Our study is to investigate characteristics and predictors of 30-day hospital readmission in patients with AML after receiving induction chemotherapy.
Methods: We analyzed the 2016 United States National Readmission Database, the latest and largest readmission database available so far. The authors identified hospitalizations for patients using ICD-10 codes for "encounter for chemotherapy" or a procedure code for administration of antineoplastic agent as the primary diagnosis with a secondary diagnosis of acute myeloid leukemia or myeloid sarcoma. We excluded patients who had a personal history of chemotherapy or those in remission or relapse in order to avoid counting patients admitted for consolidation/ re-induction chemotherapy. A readmission was defined as the first admission to any hospital for any non-traumatic diagnosis within 30 days of discharge after the index admission. Same day admissions and discharges were excluded. The primary outcome was 30-day readmission rate. Secondary outcomes were 30-day mortality rate, most common reasons for readmission, readmission mortality rate and resource utilization (length of stay and hospitalization costs). Independent risk factors for readmission were identified using multivariate regression analysis.
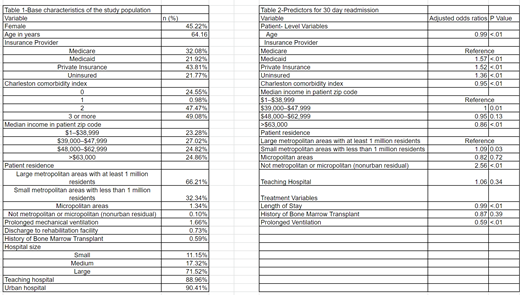
Results: A total of 18,140 admissions were identified for induction chemotherapy. The median age was 64.1 years and 45% of patients were female. The all cause 30-day readmission rates were 30.1%. The in-hospital and 30-day mortality rate were 3.9% and 4.8%, respectively. The in-hospital mortality rate for readmitted patients was 3.8%. The top five causes for unplanned readmissions were neutropenia (7.2%), sepsis (6.1%), pneumonia (2.6%), acute kidney injury (2.5%) and neoplasm related pain (2.3%). Mean total charges were higher during index admission than readmission ($118,449 vs $49,087, p=.000). Table 1 shows the base patient characteristics and Table 2 shows the odds ratios of the various factors tested as independent predictors of readmission. Independent predictors of readmission were younger age, low income, Medicaid, uninsured or Private Insurance, co-morbidities, urban hospital and length of stay during index hospitalization. The total hospital days associated with readmission were 102,924 days, with a total healthcare economic burden of $303 million.
Conclusions: Our study reveals that there is a significant readmission rate in this study population generating a substantial financial burden. 30-day readmissions are primarily due to neutropenia and infectious etiologies including sepsis and pneumonia. This emphasizes the urgent need for organizing better outpatient follow up for these patients post-hospitalization as well as increased awareness for antibiotic prophylaxis. Further research into development of clinical models for risk stratification is also required.
Rajeeve:ASH-HONORS Grant: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal