Introduction
Hemophilia is one of the most common inherited bleeding disorders. This study aims to estimate associated diagnoses, healthcare utilization, and mortality in hospitalized pediatric and adult patients with hemophilia A and B and evaluate outcome improvement trends.
Methods
The 2016 Healthcare Cost and Utilization Project's Nationwide Inpatient Sample (HCUP-NIS) was utilized for the analysis. The NIS uses a stratified probability sample of 20% of all inpatient discharges (representing more than 97% of the US population). We applied sampling weights to represent all hospital discharges for hemophilia identified using ICD-10 codes D66 and D67 and generate nationally representative estimates. For comparative historical data, we used 2007 data from a prior published study [Goel et al., Hemophilia (2012), 18, 688-692].
Results
In 2016, there were n=10,840 hospital discharges with hemophilia A or B as one of all listed diagnoses (n=1600 as principal diagnosis). Of these, 2445 were children, and 8395 were adults. The median age (interquartile range) was 52 (33-68) years for adults and 5 (1-11) years for children.
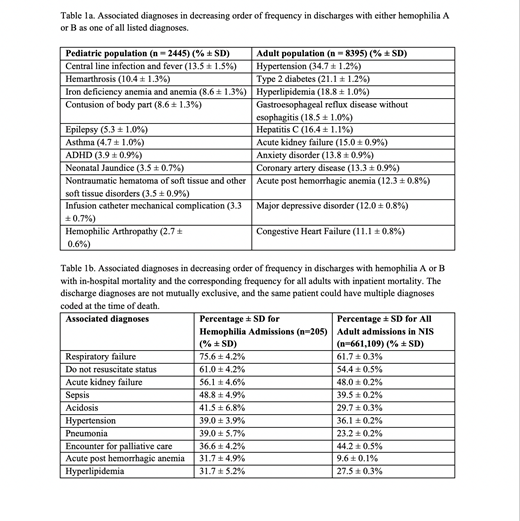
Associated Diagnoses(Table 1a)
The most common associated diagnoses in adults with hemophilia were hypertension (34.7 ± 1.2%), Type 2 diabetes (21.1 ± 1.2%), and hyperlipidemia (18.8 ± 1.0%). Other noteworthy ones include hepatitis C (16.4 ± 1.1%), coronary artery disease (13.3 ± 0.9%), and congestive heart failure (11.1 ± 0.8%). In pediatric hemophilia cases, central line infection and fever (13.5 ± 1.5%), hemarthrosis (10.4 ± 1.3%), and anemia (8.6 ± 1.3%) were the most common discharge diagnoses. HIV/AIDS and hepatitis C were not reported in children and listed in 5.9 ± 0.6% and 16.4 ± 1.1% of adults, with the youngest age at reported diagnosis being 32 and 21 years, respectively.
Mortality(Table 1b)
The all-cause in-hospital mortality was 1.9% for hemophilia related admissions, which was comparable to all NIS hospitalizations at 1.9%. The median age at death in years (interquartile range) for hemophilia patients was 72 (57-78) and comparable to 73 (61-83) for all hospitalizations. The most common diagnoses associated with mortality included respiratory failure, "do not resuscitate" status, and sepsis. There was no inpatient mortality reported in children, and the youngest age for in-hospital death was 27 years.
Health Care Utilization
96.0% of all hemophilia admissions had insurance coverage with the distribution as follows: Medicare: 33.4%, Medicaid: 28.8%, private insurance: 28.6%. For all NIS hospitalizations, 96.1% had coverage (Medicare: 39.6%, Medicaid: 23.1%, private insurance: 30.1%). The median hospital stay length per hemophilia admission was 3 days (2-6) and was similar to all hospital stays at 3 days (2-5). The median hospital charge per hemophilia admission was $50,662 as compared to $25,261 for all hospital admissions.
2007 Comparison
When we compared our data to 2007, serving as a near-decade long follow-up, insurance distribution, inpatient mortality rate, and length of stay were relatively unchanged. Amongst the most common diagnoses for adults with hemophilia were hypertension (up from 28.1% to 34.7%), hepatitis C (down from 21.8% to 16.4%), congestive heart failure (up from 8.1% to 11.1%), and HIV/AIDS (stable at 5.6% and 5.9% respectively). In both 2007 and 2016, there were no HIV or hepatitis C cases amongst children with hemophilia. Notably, in 2007, there were more bleeding related diagnoses, such as hematuria and hemorrhages. There was no inpatient mortality for children in 2016, while there were 15 day of life zero deaths (7% mortality rate) in 2007. The median age at death was also greater in 2016 (72 and 68.3 years).
Discussion/Conclusions
Adult hemophilia hospitalizations were in large part related to non-bleeding complications and age-related co-morbidities. In contrast, catheter-related infections and bleeding remain the top reasons for pediatric admissions. Most hemophilia patients had insurance coverage. The median hospital charge for those with hemophilia was nearly twice that of all-cause hospitalizations. Advancements in hemophilia treatment and outcomes are continuing, as evidenced by the improved mortality rate and median survival range approaching those from all hospitalizations. These changes all cumulatively demonstrate significant treatment and health care advancements in hemophilia management.
Takemoto:Genetech: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Other: DSMB for aplastic anemia trial.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal