Introduction: Hepatic veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) is a potentially fatal complication that occurs after hematopoietic cell transplantation (HCT) and may also develop after high-dose chemotherapy alone. The reported incidence of VOD/SOS post-HCT has been estimated to be 14% (Coppell JA, et al. Biol Blood Marrow Transplant. 2010;16:157-168). In a study that defined severe VOD/SOS as the presence of multi-organ failure, the total medical costs per patient with severe VOD/SOS have been reported to be higher than those without severe disease (Zhang X, et al. Clin Ther. 2018;40:1711-1719). A previous retrospective study (Premier I), which evaluated patients from the Premier Healthcare Database (2009-2014) in the absence of formal diagnostic codes for VOD/SOS, reported an incidence of VOD/SOS of 5.3% and 6.3% in adult and pediatric patients, respectively (Cao Z, et al. J Med Econ. 2017;20:871-883). This study (Premier II) developed an algorithm to identify cases of VOD/SOS using ICD-10-CM diagnostic codes to evaluate health resource utilization, costs, and outcomes in patients with VOD/SOS post-HCT, with and without multi-organ dysfunction (MOD), compared to patients with no VOD/SOS.
Methods: This retrospective, observational study used data from the Premier Healthcare Database and included patients with an inpatient hospitalization from October 2015 through January 2018 for HCT (identified by ICD-10-CM/PCS codes, CPT, HCPCS, or MS-DRG). VOD/SOS patients were identified by an algorithm based on clinical experience, which utilizes ICD-10-CM diagnostic code K76.5, other diagnosis codes for VOD/SOS-related clinical manifestations, or evidence of defibrotide use within 90 days following index hospitalization (ie, first hospitalization). VOD/SOS patients who also had diagnosis or procedure codes for MOD in the same hospitalization or visit comprised the VOD/SOS with MOD group. VOD/SOS patients without evidence of MOD comprised the VOD/SOS without MOD group. Patients with HCT but without evidence of VOD/SOS comprised the no VOD/SOS group. Patients aged ≥18 years were considered adults. Total hospital length of stay (LOS) and total costs were examined during index hospitalization and the 90 days following index discharge (ie, discharge from the index hospitalization stay). Bivariate analysis was performed to examine the difference in unadjusted outcomes between post-HCT patients with VOD/SOS and those without VOD/SOS. The Wilcoxon test was used for continuous variables, and the Chi-square test was used for categorical or dichotomous variables. An adjusted analysis based on multivariable regressions was used to control for patient and hospital characteristics.
Results: The analysis included 4,642 patients with HCT and a qualifying discharge (no VOD/SOS: n = 4,352; VOD/SOS with MOD: n = 177; VOD/SOS without MOD: n = 113). Overall, VOD/SOS occurred in 6.2% of patients; 3.8% and 2.4% of patients had VOD/SOS with and without MOD, respectively. VOD/SOS was more common in pediatric (14.3%) than adult (5.7%) patients and in patients with allogeneic (11.4%) versus autologous HCT (3.5%).
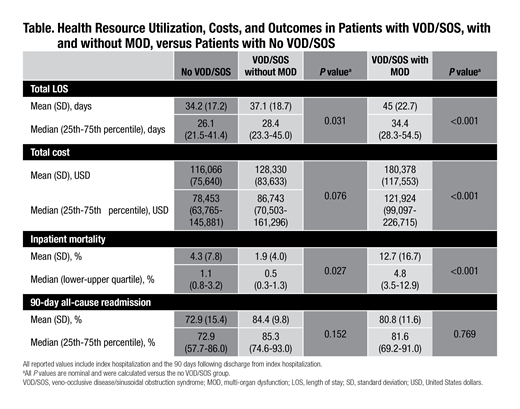
Regression-adjusted total hospital LOS in the 90-day follow-up period was longer both in patients with VOD/SOS with MOD and in patients with VOD/SOS without MOD, compared to patients with no VOD/SOS (Table). Compared to no VOD/SOS patients, adjusted total costs during follow-up were higher in patients with VOD/SOS with MOD (Table). Adjusted inpatient mortality in the 90-day follow-up period was higher for patients with VOD/SOS with MOD compared to patients with no VOD/SOS (Table). The difference in the rate of 90-day, all-cause readmission was not statistically significant across groups (Table).
Conclusions: The results from this retrospective study using the Premier Healthcare Database are consistent with rates of VOD/SOS reported in the literature and in Premier I. This indicates that, although the incidence of VOD/SOS has declined over the years, the risk of VOD/SOS remains. The slightly higher rate of VOD/SOS reported here versus in Premier I was driven by a higher incidence in pediatric and allogeneic populations. The presence of VOD/SOS, especially VOD/SOS with MOD, in post-HCT patients was associated with increases in healthcare resource utilization, LOS, and costs compared to HCT patients without VOD/SOS.
Dvorak:Alexion Inc: Consultancy; Jazz Pharmaceuticals: Consultancy. Cao:Premier Inc.: Employment, Other: Premier received funding from Jazz Parmaceuticals to perform the study and analysis; Jazz Pharmaceuticals: Other: Zhun Cao is an employee of Premier Inc, which receives payments from Jazz Pharmaceuticals for this research project.. Price:Jazz Pharmaceuticals: Employment, Equity Ownership. Coaquira:Jazz Pharmaceuticals: Employment, Equity Ownership. Lipkin:Premier Inc.: Employment, Other: Premier received funding from Jazz Pharmaceuticals to perform the study and analysis. Robinson:Premier Inc.: Employment, Other: Premier received funding from Jazz Pharmaceuticals to perform the study and analysis; Jazz Pharmaceuticals: Other: Scott Robinson is an employee of Premier Inc, which receives payments from Jazz Pharmaceuticals for this research project.. Kebriaei:Jazz: Consultancy; Amgen: Research Funding; Pfizer: Honoraria; Kite: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal