Background: The field has made significant strides in understanding the mechanisms underlying pediatric sickle cell disease (SCD), and the coming years will likely see the approval of several new medications to treat SCD. The impact of these medications on clinical outcomes, however, will be dependent on patient adherence. Adolescents with SCD are at particular risk for non-adherence, and as disease management increasingly includes self-administration of oral medications, adherence assessment will become a critical component of research on medication effectiveness and clinical care. While electronic monitoring devices (bottles with computer chips that record date- and time-stamps of device openings) such as MEMS® bottles are considered the "gold standard" for adherence assessment in other populations, their feasibility among adolescents with SCD remains unknown.
Objectives: The primary aims of this study were to examine data on MEMS® bottle use among adolescents (ages 13-21 years) with SCD to: 1) evaluate the feasibility of MEMS® bottle use; and 2) elicit barriers and facilitators to MEMS® bottle use.
Methods: As part of a larger study of a self-management intervention, adolescents were asked to use a MEMS® bottle to store and administer their daily oral medication (hydroxyurea or deferasirox) for the 18-week study duration. The larger study included baseline, post-treatment, and follow-up assessments, at which adolescents were asked to provide their MEMS® bottle for data download. Descriptive statistics were calculated to assess multiple domains of MEMS® bottle feasibility including: initial uptake (% enrolled), MEMS® initiation (% initiated), and MEMS® sustained use (% completed; % provided bottles for download ±2 weeks of scheduled study visit = "on time"). Barriers and facilitators to MEMS® use were elicited via adolescent self-report.
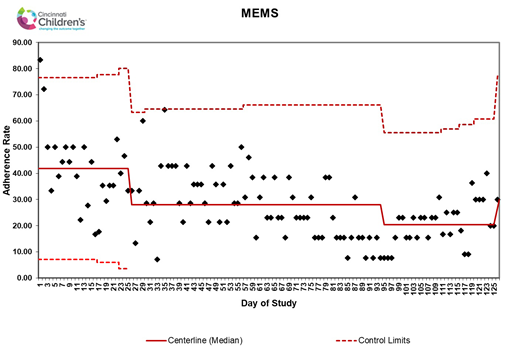
Results: In the larger study, 18 non-Hispanic African-American adolescents (M = 17.8 years, SD = 2.6; 61% male) with HbSS were asked to use a MEMS® bottle to store their hydroxyurea (n = 14) or deferasirox (n = 4). Initial uptake was 94.7%, with 18 of 19 eligible adolescents enrolling in the study. Of the 18 enrolled adolescents, all initiated MEMS® use (100%) and 11 sustained MEMS® use through the final study endpoint (61.1%). Eight (44.4%) and 2 (11.1%) adolescents provided their MEMS® bottle for download "on time" at post-treatment (42 days) and follow-up (126 days), respectively. Barriers to MEMS® use included medication changes (i.e., medication holds, dose timing changes) and transitioning from pediatric to adult care. Facilitators included tip sheets (e.g., places to store bottle, reminder to place refills in bottle) and reminder calls. Participants took a median of 26.2% of doses using the MEMS® across the 126 days (SD = 22.4; range 0.79% - 79.3%), illustrating that electronic monitoring devices are not a solution to medication adherence, but are one component of an adherence support strategy. See Figure 1 for adherence rates over time.
Discussion: Data suggest that MEMS® are acceptable to adolescents with SCD. Ensuring sustained MEMS® use, however, will likely require additional supports. For example, electronic monitors which automatically transmit data in real-time via Bluetooth or cellular connections would eliminate the need for adolescents to bring bottles to study visits for data downloads. Researchers and clinicians interested in using electronic monitoring devices are encouraged to consider remote monitoring capabilities along with other device features when selecting a product. Larger studies are needed to evaluate concordance between rates of adherence obtained via electronic monitoring and other assessments and to validate electronically-monitored medication adherence with clinically-relevant outcomes for adolescents with SCD.
Quinn:Celgene: Membership on an entity's Board of Directors or advisory committees; Amgen: Other: Research Support.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal