
Introduction
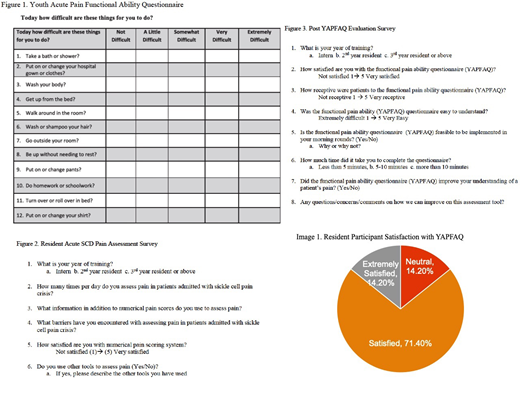
Acute vaso-occlusive pain crises are the most common complications of sickle cell disease (SCD). Pain is a subjective sensation and is often difficult to describe and for practitioners to understand. The complexity and multidimensional nature of pain requires additional evaluation beyond pain intensity. Pain assessment is also influenced by implicit and explicit biases related to race and ethnicity which can negatively influence treatment (Wandner et al J Pain 2012). In this pilot quality improvement study, we studied resident perceptions to a functional assessment tool in adult patients hospitalized with sickle cell vaso-occlusive crises. We used the Youth Acute Pain Functional Ability Questionnaire (YAPFAQ), a validated questionnaire of physical function in youth experiencing acute pain (Zempsky et al J Pain 2014) (Figure 1). Resident responses to using the YAPFAQ were measured as an initial step to implementation of functional pain assessment in hospitalized adults with SCD pain crises.
Methods
We piloted this study on internal medicine residents. First, residents completed the Resident Acute SCD Pain Assessment Survey regarding their current management of acute pain in SCD (Figure 2). This was done to determine their baseline demographic information, methods of pain assessment, satisfaction with the numerical pain score system, and to understand barriers in assessing acute pain. This survey included a combination of multiple choice, free response, and binary response options. The residents then trialed the YAPFAQ with a patient admitted with vaso-occlusive pain crisis then the residents completed The Post YAPFAQ Evaluation Survey in response to this assessment tool (Figure 3). This survey included a combination of multiple choice, free response, and binary response options. The goal of this survey was to assess resident satisfaction with YAPFAQ, perceived patient receptiveness to YAPFAQ, and feasibility of using this tool during daily assessments. Patients were not surveyed during this pilot study. We performed descriptive statistics to describe the survey results.
Results
Sixteen residents completed the Acute SCD Pain Management survey prior to using the YAPFAQ. Sixty-nine percent of residents reported dissatisfaction with using numerical pain scores. Reported barriers to assessing pain included: subjectivity of pain scores, concern for malingering, and the ceiling effect of the numeric scale. Seven residents completed the post YAPFAQ evaluation survey. A majority of residents (86%) were extremely satisfied or satisfied with using the YAPFAQ. Fifty seven percent of residents felt that patients were extremely receptive or receptive to using this tool. The majority of residents (85%) felt that the YAPFAQ improved their understanding of patients' pain. All YAPFAQs were completed with patients in 10 minutes or less. Most residents (57%) reported that the tool would be feasible for implementation on rounds.
Conclusions
Similar to previous studies, our residents felt that numerical pain score systems inadequately describe pain. Residents had generally positive responses to the YAPFAQ. One resident stated that the questionnaire was "structured and easy to compare day to day." Functional pain assessment allows providers to better understand how pain limits daily activities and can provide useful functional targets for safe hospital discharge. Future directions of this project include performing a larger study of patients hospitalized with vaso-occlusive pain crises to validate the YAPFAQ in adult patients, survey patients regarding experiences with the YAPFAQ, and to create tailored pain management plans based on functional pain assessments.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal