Introduction
Sickle cell disease (SCD) affects over 100,000 people in the US, the majority of whom are African American. Socioeconomic challenges have a significant impact on both access and adherence to appropriate treatments which, given a history of racial segregation and discrimination, disproportionately burden under-represented minorities. The distribution of socioeconomic factors, like poverty, educational attainment, and housing quality, can now be assessed routinely at the population level, yet the distribution and impact of such contextual risks in the pediatric sickle cell population have not been sufficiently described. Here, we sought to characterize the burden of neighborhood-level socioeconomic challenges and barriers among children with SCD in one large, urban county. We also sought to determine whether these area-level indicators were associated with hospitalizations and markers of adherence to SCD medications.
Methods
We pursued a retrospective review of electronic health record data from 2011-2017 for children with HbSS disease in the active Cincinnati Children's Hospital Medical Center's SCD registry which includes all children receiving care within the past two years in the Comprehensive Sickle Cell Center and is representative of nearly all children with SCD in Hamilton County, Ohio. The analysis was performed under an IRB-approved study investigating socioeconomic factors for children in Hamilton County. Children within the SCD registry were excluded from this analysis if they had a non-HbSS genotype or an address outside of Hamilton County. Addresses were geocoded and linked to a specific census tract which approximates local neighborhood boundaries. Once linked to a census tract, that address was connected to a pre-determined list of variables present within the 2013-2017 US Census' American Community Survey. Variables included the census tract poverty rate, educational attainment rate (percentage of adults with less than a high school education), and the percentage of vacant housing. A validated census tract-level deprivation index, assembled from 6 such census variables, was also included. Outcomes of interest included number of hospitalizations and ED visits during the study period and %HbF for the subset on hydroxyurea treatment. Descriptive statistics were used to illustrate ecological socioeconomic characteristics among included patients. Associations between area-based socioeconomic deprivation and outcomes of interest were tested using the Kruskal-Wallis Test.
Results
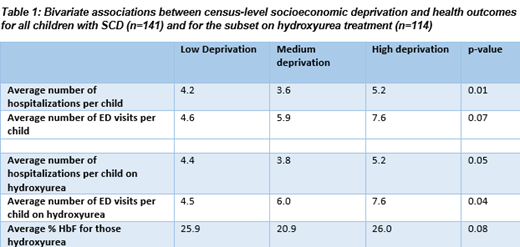
There were 141 patients with HbSS included in the analysis (53% Male, 82% publicly insured). Mean age at the end of the analysis period was 9.6±6.3 years. Consistent with the aggressive treatment strategy at our center, most (97%) were on disease modifying treatment with either hydroxyurea (81%) or chronic transfusion therapy (16%). Compared to the county as a whole, children in the registry mapped to areas with relatively high rates of poverty (median 26%; IQR 15%-42%), low rates of education attainment (median with high school degree 86%; IQR 78%-91%), and high rates of vacant housing (median 13%; IQR 8%-19%). The deprivation index is scaled between 0 and 1 with higher values indicative of more socioeconomic deprivation. In our population, the deprivation index median was 0.45 (IQR 0.36-0.61). When the sample was categorized into three deprivation groups (low < 25th percentile, medium between 25th and 75th, and high >75th percentile), we found trends toward associations with utilization and adherence measures (Table 1).
Conclusion
A majority of our SCD patients live in neighborhoods with stark socioeconomic challenges and barriers which have been shown to negatively affect health outcomes. There appears to be a significant trend towards increased utilization among those living in more deprived neighborhoods, although, the link with adherence was less clear. The latter finding, indicative of similar HbF levels across deprivation groupings, may be the result of efforts made by our multidisciplinary comprehensive care team to optimize care for all patients regardless of socioeconomic challenges. The data presented here are novel and likely representative of socioeconomic challenges of most SCD patients living in the US. Future, larger, multi-center studies should focus on identifying and addressing social determinants of health within this population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal