BACKGROUND: Venous-thromboembolism (VTE) is a debilitating condition and is associated with excess mortality. Small, single institution studies suggest that the risk of VTE in acute myeloid leukemia (AML) patients is elevated and is similar to that seen in solid tumor patients. However, population-based studies describing VTE risk and predictors of VTE in elderly AML patients are lacking. We used Medicare-linked SEER (Surveillance, Epidemiology, and End Results) data to address this knowledge gap.
METHODS: We identified 4,166 Medicare beneficiaries diagnosed with AML at age ≥67y between 2007 and 2013. We ascertained baseline sociodemographics and pre-existing comorbidities for 2y prior to AML diagnosis. Patients were followed from AML diagnosis until development of post-AML VTE, or, in the absence of VTE diagnosis, for 2y (if alive), or until death, blood or marrow transplant, or end of study (12/31/2014), whichever came first. VTE diagnosis was based on ICD 9 codes using validated claims algorithms, and included deep vein thrombosis (DVT), pulmonary embolism (PE) and thrombophlebitis. Statistical Analysis: Cumulative incidence functions were used to assess post-AML VTE risk (overall, new-onset). Cox regression models examined the following risk factors associated with VTE: age at AML diagnosis, sex, race/ethnicity, socioeconomic status, history of pre-AML VTE, and pre-existing co-morbid conditions (hypertension, dyslipidemia, diabetes, stroke, rheumatoid arthritis, ischemic heart disease, chronic obstructive pulmonary disease, chronic kidney disease, congestive heart failure, atrial fibrillation, anemia and peripheral vascular disease).
RESULTS: Median age at AML diagnosis was 79y (range: 67-105y); 52% were male, 83% non-Hispanic white and 20% resided in an area where >20% of the population lived below poverty level; 50% of the cohort received chemotherapy. Prior to AML diagnosis, 15% were receiving anticoagulants; 2% were on anticoagulation for pre-AML VTE.
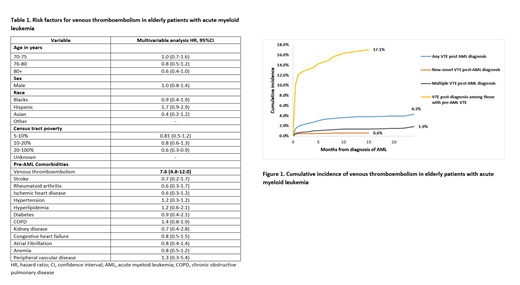
Cumulative Incidence of VTE: Overall, 167 (4.0%) patients were diagnosed with post-AML VTE (DVT [63%], PE [32%], thrombophlebitis [5%]); 38% had >1 VTE. Of the 167 patients with post-AML VTE, only 25 (15%) had new-onset VTE; the remaining 142 carried a history of pre-AML VTE. The 2y cumulative incidence of any post-AML VTE was 4.3% (95%CI: 3.6%-5.1%) (Fig 1). Fifty-six percent of VTE episodes occurred within 3 months of AML diagnosis. The incidence was 0.6% (95% CI: 0.5%-0.8%) for new-onset VTE and was 1.9% (95%CI 1.3-2.6) for multiple VTEs. The 2y cumulative incidence of post-AML VTE among those with a history of pre-AML VTE was 17.1% (95% CI: 13.3-21.9%).
Risk factors for VTE: Adjusting for age at diagnosis, race/ethnicity, census-tract poverty, and co-morbid conditions, AML patients who had pre-AML VTE, were at 7.6-fold increased risk of post-AML VTE (95%CI: 4.8-12.0, p<0.001). No other risk factors were associated with post-AML VTE risk, with the exception of a marginal association between a prior history of peripheral vascular disease and new-onset VTE (HR=3.5, 95%CI: 0.9-14.8, p=0.08) (Table 1).
Risk factors for VTE among patients receiving chemotherapy: Adjusting for age at diagnosis, race/ethnicity, census-tract poverty and co-morbid conditions, AML patients with pre-AML VTE were at 8.1-fold increased risk of any post-AML VTE (95%CI: 4.4-14.7, p<0.001).
Mortality associated with VTE: The 2y cumulative incidence of mortality for those with no pre-AML VTE was 91%, compared to 95% for those with a pre-AML VTE (HR 1.23, p=0.017). New-onset VTE after the diagnosis of AML was not associated with an increased risk in mortality (HR 1.04, p=0.705).
CONCLUSION: History of VTE prior to diagnosis of AML significantly increases the risk of post-AML VTE and overall mortality. These findings can be used to inform appropriate thromboprophylaxis in elderly AML patients who carry a pre-AML diagnosis of VTE.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal