
Introduction: During transition from pediatric to adult care, young adults with sickle cell disease (SCD) experience increased acute healthcare utilization and mortality. Functional transitional programs maintain care quality; however, there is a dearth of program outcomes concerning adult care retention. The St. Jude Transition to Adult Care Program is embedded within a co-located medical home for SCD spanning the ages of 12-25 years. The co-location model bridges pediatric and adult care at three levels: (1) hematology provider (2) neuropsychologist and (3) transition nurse coordinator. Previous work demonstrated that young adults who receive care within a co-located transition model of care do not have the typical increase in acute care utilization during transition (Nolan, AJH 2017). Here, we tested the hypothesis that individuals who participated in the co-location model until age 25 years have greater retention in adult care 12- or 24- months after engaging in adult care, compared to those who only received pediatric co-location transition services (until age 18). Further, we explored adult environmental factors as predictors of retention in adult care at 12- and 24- months.
Methods: With IRB approval, we analyzed the outcomes of participants of the longitudinal cohort study Sickle Cell Clinical Research and Intervention Program (SCCRIP, PBC 2018), who completed transfer from pediatric to adult care from January 2007 to December 2017. Participants were excluded if they did not have enough time in adult care for the 12- and 24-month retention analysis. Adult care retention was defined as continuation with the same provider for ≥12 or ≥24 months post-pediatric care and was compared among adults who transferred to adult care within the co-location model vs. those who did not. Chi-square tests were used to test associations between demographics and co-location model exposure. Logistic regression estimated the association between care abandonment (defined as voluntarily discontinuing pediatric care or dying before 12- or 24- months from initiating adult care) and co-location status at 12- and 24- months. Each model was tested for effect modification and confounding by the following variables: sex, genotype, year of last pediatric visit, and age at transfer. Fisher's Exact Test investigated predictors of adult care retention within the adult co-location model including employment status, education level, crowding, marital status, household income, and health insurance status during the first year of adult care. P-values <0.05 were significant.
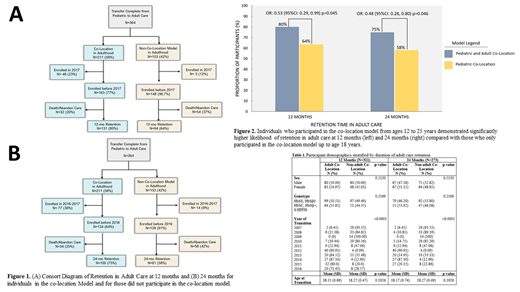
Results: Of the 364 patients who transferred to adult care, 211 (58.0%) participated in the transition co-location model. Fifty-three (14.5%) individuals were excluded from the 12-month analysis due to having <12 months of adult care opportunity (Figure 1A). Of the 311 participants included (51.5 % male; 63% HbSS/HbSβ0-thalassemia), the median age at last pediatric visit was 18 years (range 13 to 20). There was a significant difference in exposure to each transition model based on year of adult care transfer (Table 1). Those in the co-location model had a 47% significantly decreased odds of abandoning care within 12 months of transfer to adult care when compared to those in the non-co-location model when controlled for year of last pediatric visit (Figure 2; p=0.045). There were 91 (25%) individuals excluded from the 24-month analysis due to having <24 months of adult care opportunity (Figure 1B). Of the 273 participants included (52.01% male; 62.64% HbSS/HbSβ0-thalassemia), those within the co-location model until age 25 years had 52% significantly decreased odds of abandoning care within 24 months of transfer to adult care when compared to those in the co-location model in childhood only. (Figure 2; p=0.046). Exclusion of individuals who died yielded similar findings relative to the duration of co-location exposure and adult care retention. Within the adult co-location model, environmental factors were collected on 31 adults (median age 22 years, range 20-26). Participants who transfer earlier (17 vs. 18 years) was predictive of less attrition at 24 months (p= 0.014). No other environmental factors were significant.
Conclusion: Continuity of providers from pediatric to adult care may increase long-term retention in adult care. Longitudinal monitoring of adult outcomes is critical to identifying the efficacy of transition services.
Ataga:Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Global Blood Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Emmaus Life Sciences: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bioverativ: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Research Funding; Modus Therapeutics: Honoraria. Hankins:ASPHO: Honoraria; NHLBI: Honoraria; National Committee for Quality Assurance: Consultancy; Global Blood Therapeutics: Research Funding; NHLBI: Research Funding; LYNKS Foundation: Research Funding; Novartis: Research Funding; Bluebird Bio: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal