Background: Over the years, splenectomy has dropped out of favor as a treatment option for Immune Thrombocytopenic Purpura (ITP) and is now considered only for patients who have failed multiple lines of therapy. One of the major concerns is surgical morbidity. We aim to study in-hospital outcomes following elective splenectomy in this population
Methods: This is a retrospective cohort analysis of NIS database (years 2006 to 2014). Patients ≥18 years of age, who had an elective admission associated with International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) procedure code for splenectomy were included in the study. Our cohort of interest was patients with ITP who underwent elective splenectomy (ITP ES). ICD-9-CM diagnosis codes were used to identify patients with ITP. All other patients who underwent elective splenectomy were labeled as non-ITP ES. Utilization of intensive care services was identified by procedure codes associated with vasopressor use, cardiopulmonary resuscitation, mechanical ventilation and initiation of dialysis in the absence of pre-existing end stage renal disease. Primary outcome was inpatient mortality and secondary outcome was length of stay (LOS). Associated factors were analyzed using multivariate logistic regression analysis. A p-value <0.05 was considered significant. We used STATA for statistical analysis.
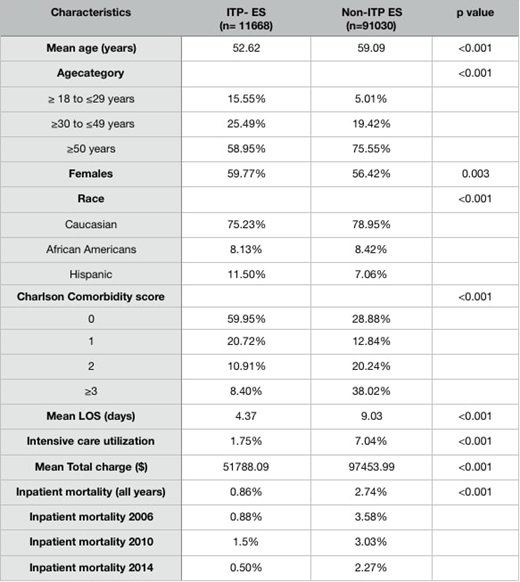
Results: A total of 102,698 admissions for elective splenectomies (ES) in adults were identified between the years 2006 and 2014,of which 11.36% (n= 11,668) were ITP ES. Inpatient mortality and mean LOS for all patients undergoing ES was 2.53% and 8.51 days respectively. Inpatient mortality and mean LOS in the ITP ES cohort was 0.86% and 4.37 days respectively. In the entire cohort of ES, inpatient mortality was lower in those with ITP versus non-ITP (OR 0.36, p<0.001). Also females had lower mortality when compared to men (OR 0.50, p<0.001). Inpatient mortality was higher with increasing age (OR 1.03, p<0.001) and Charlson Comorbidity Index (CCI) ≥3 vs 0 (OR 1.54, p <0.001). Mean length of stay was lower in those with ITP vs non ITP by 3.3 days (p<0.001). Within the ITP-ES cohort, mortality was higher with increasing age (OR 1.12, p <0.001), CCI ≥3 vs 0 (OR 18.39, p< 0.0001) and CCI 2 vs 0 (OR 8.61, p 0.008). Inpatient mortality was lower in teaching hospitals compared to non-teaching hospitals with a trend towards significance (OR 0.35, p 0.05). Gender, insurance status, income quartile, geographic region and hospital size did not affect odds of inpatient mortality in this cohort. Length of stay (LOS) in ITP ES cohort had positive correlation with age (coefficient 0.038, p<0.001), income quartile 51-75th vs 0-25th percentile (coefficient 0.81, p 0.03), CCI ≥3 vs 0 (coefficient 3.29, p<0.001), CCI 2 vs 0 (coefficient 2.11, p<0.001), CCI 1 vs 0 (coefficient 0.86, p<0.001). There was no association of gender, insurance status and geographic region with LOS within this cohort.
Conclusion: Inpatient mortality and length of stay in admissions for elective splenectomy was significantly lower in ITP patients compared to non ITP patients. Also, in ITP patients undergoing elective splenectomy, older age and a charlson comorbidity index of 2 or above were associated with higher odds of dying in the same admission.These findings from real world data have practical implications for clinicians and patients, as they weigh the pros and cons of splenectomy as a treatment option for ITP.
Donthireddy:Viracta: Other: PI for Clinical Trial.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal