Background:
The use of mismatched unrelated (MMUD) donor grafts in leukemic patients who are in need of allogeneic hematopoietic cell transplantation (HCT) and do not have a fully matched donor, represents an alternative therapeutic option. Data on HCT outcome after ≤6/8 MMUD are limited.
Methods:
We used the data set of the acute leukemia working party (ALWP) of the European society of blood and marrow transplantation (EBMT) in order to assess the transplantation outcome in patients (pts) with acute myelogenous or lymphoblastic leukemia (AML/ALL) transplanted from ≤6/8 MMUD (2-4 HLA mismatches at the allelic level at loci A, B, C and DR) in remission (CR), with no ex vivo T cell depletion (TCD). HCT were performed between 2000 and 2017. Multivariate analyses (MVA) were performed using the Cox proportional hazard model.
Results:
The study population consisted of 465 patients who met the inclusion criteria (AML 320, ALL 145). The median age at transplantation was 50.2 years (range, 18-71.8) and 34.8 years (range, 18.2-62.9); 54% and 64% were males in AML and ALL groups, respectively. Median follow up was 63 and 75 months, respectively. 69% and 66% were in CR1, while 31% and 34% were in CR2. 40% of AML pts had intermediate risk cytogenetics, 10% poor risk and 5% good risk (missing -45%), respectively. 37% of ALL pts were Ph positive, 22% Ph negative and 18% T ALL (17% B ALL with no Ph data, 6% missing immunophenotyping data). The number of HLA mismatches (HLAMM), it was 6/8 HLA MM - in 82% and 85%, 5/8- in 11.5% and 12% and 4/8- in 6% and 3% of AML and ALL pts, respectively. 85% of AML pts and 77% of ALL pts received PBSC graft. The conditioning regimen was myeloablative in the majority of patients (89% of AML and 61% of ALL pts). 82% and 77% underwent in vivo TCD, respectively. Graft versus host disease (GVHD) prophylaxis was CSA/MTX in 51% and 67% and CSA/MMF in 21% and 10% of AML and ALL pts, respectively. Engraftment was achieved in 97% and 95% of pts, respectively. The incidence of acute (a) GVHD grade (Gr) II-IV and Gr III-IV was 34% and 41% and 14% and 21% for AML and ALL pts, respectively.
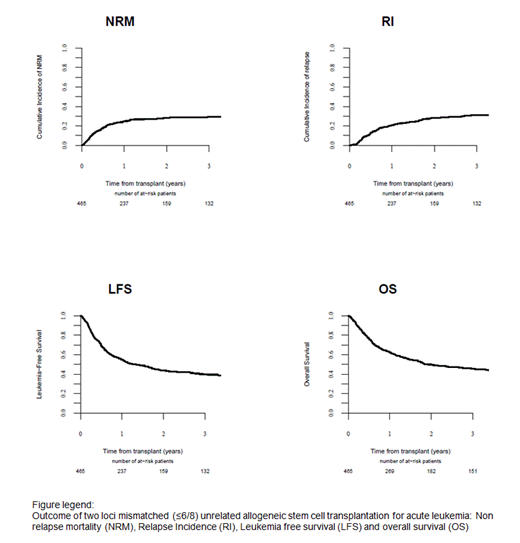
Total and extensive chronic(c) GVHD rates at 2y were 38% and 38% and 23% and 14%, respectively. The main causes of death were disease recurrence (37% in both), GVHD (29% and 22%) and infections (22% and 26%). In the entire population, 2 and 5y outcomes were: relapse incidence (RI) -28% (95% CI: 24 - 32) and 33% (95% CI: 28 - 37), non-relapse mortality (NRM)- 28% (95% CI: 24 - 32) and 30% (95% CI: 26 - 35); leukemia free survival (LFS) -44 % (95% CI: 39 - 48) and 37 % (95% CI: 32 - 41 ), overall survival -50% (95% CI: 45 - 55 ) and 41% (95% CI: 36 - 46) and GVHD free relapse free survival (GRFS)- 33% (95% CI: 29 - 38) and 27% (95% CI: 22 - 31), respectively. More than 2 HLA mismatches were associated with a higher incidence of aGVHD Gr II-IV (29% vs 15%, respectively).
In MVA, RI was lower for ALL vs AML HR (95% CI) 0.60 (0.39-0.93), p=0.02. Disease status (CR2 vs CR1) was poor prognostic factor for RI, LFS and OS. Age was prognostic factor for NRM, LFS and OS. HLA- mismatch at locus DR was poor prognostic factor, giving increased NRM: HR (95% CI) 1.68 (1.1-2.5), p=0.02, and lower LFS: HR (95% CI), 1.42 (1.03-1.95), p= 0.03 and OS HR (95% CI) 1.46 (1.04-2.03), p=0.03 and higher GVHD Gr II-IV HR (95% CI) 1.48 (1-2.17), p= 0.048. Results of MVA in AML pts in CR1 were similar. GVHD prophylaxis with CSA/MMF in comparison to CSA/MTX resulted in higher NRM HR (95% CI) 2.2 (1.27-3.82), p=0.005 and lower GRFS HR (95% CI) 1.58 (1.06-2.35), p= 0.02.
Notably, in 154 pts with AML in CR1 transplanted from 6/8 UD with in vivo TCD, C mismatches was associated with higher incidence of cGVHD, HR (95% CI) 2.52 (1.40-4.53), p= 0.002.
Conclusions:
HCT from ≤6/8 MMUD is an alternative transplantation option for acute leukemia pts in CR that can provide 40% 5y OS, 37% LFS and GRFS of 27%. DR mismatch is a poor prognostic factor. cGVHD incidence at 5y was 41% with 21% being severe and is associated in AML pts with HLA C mismatches. CSA and MTX is the preferred GVHD prophylaxis. Emerging novel agents will hopefully reduce the incidence of cGVHD in the near future and thus improve HCT from ≤6/8 MMUD outcome.
Rambaldi:Italfarmaco: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Research Funding, Speakers Bureau; Omeros: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Speakers Bureau; Roche: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Research Funding, Speakers Bureau; Amgen: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Research Funding, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Other: travel support, Speakers Bureau; Jazz: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Socie:Alexion: Consultancy. Mielke:Celgene: Honoraria, Other: Travel support (via institution), Speakers Bureau; EBMT/EHA: Other: Travel support; Bellicum: Consultancy, Honoraria, Other: Travel (via institution); IACH: Other: Travel support; Jazz Pharma: Honoraria, Other: Travel support, Speakers Bureau; DGHO: Other: Travel support; Kiadis Pharma: Consultancy, Honoraria, Other: Travel support (via institution), Speakers Bureau; GILEAD: Consultancy, Honoraria, Other: travel (via institution), Speakers Bureau; ISCT: Other: Travel support; Miltenyi: Consultancy, Honoraria, Other: Travel and speakers fee (via institution), Speakers Bureau. Platzbecker:Celgene: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Novartis: Consultancy, Honoraria. Finke:Riemser: Honoraria, Other: research support, Speakers Bureau; Neovii: Honoraria, Other: research support, Speakers Bureau; Medac: Honoraria, Other: research support, Speakers Bureau. Mohty:Jazz Pharmaceuticals: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal