
Introduction
The advanced refractory/relapsed acute leukemia has a very dismal prognosis even with the salvage allogeneic hematopoietic stem cell transplantation (allo-HSCT). To develop a novel transplant protocol to achieve a rapid engraftment and quick graft-versus leukemia (GVL) effect is crucial. Based on previous observation, the G-CSF primed bone marrow (BM) plus peripheral blood mononuclear cells (PBMNCs) could not only increase mononuclear cells and CD34 cells, but also change T-cell biology by down-regulating the expression of adhesion and CD28/B7 molecules and increase the absolute number of D2APCS, which promotes a T-cell shift from T1 to T2 subset to secrete a higher anti-inflammatory cytokines of IL-4 and IL-10. After going through a rigorous conditioning, the recipients' T-cells are incapable to attack host. We propose that reinfusion of G-CSF primed donor PBMNCs to recipient on transplant day + 6 may cross mismatched MHC barrier thus accelerating engraftment.
Patients and Methods
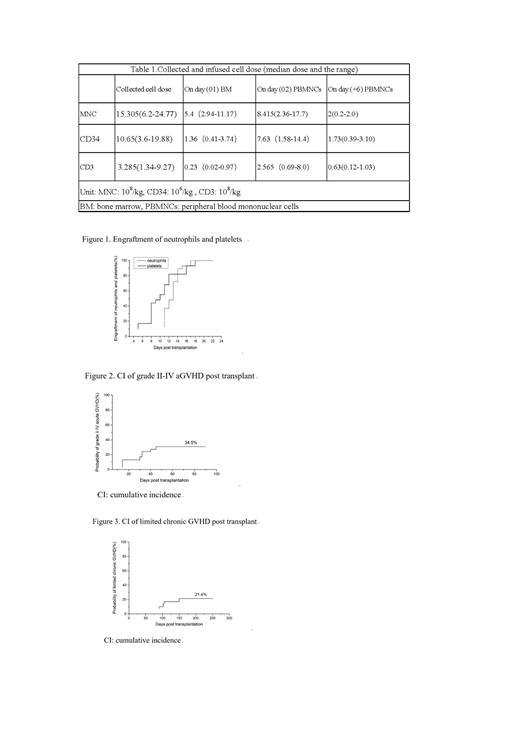
From April 2018 to June 2019, 30 advanced-stage patients with refractory/relapsed acute leukemia were enrolled and underwent a salvage haploidentical (haplo)-HSCT. The median age was 12 (2-63) years with M/F ratio of 17/13. There were 21 patients with acute myelocytic leukemia (AML, 70%), 4 -cell acute lymphoblastic leukemia (B-ALL, 13%), 2 biphenotypic acute leukemia (BAL, 7%), 1 juvenile myelomonocytic leukemia (JMML, 3%), and 2 T-lymphoblast leukemia (T-LBL, 7%). The median BM blasts were 40% (5%-90%). Twenty-eight patients received a conditioning regimen including fludarabine 30mg/m2/d×4 day, cytarabine 2.0g/m2/d×4 days, busulfan 3.2mg/kg/d Q6h×4days, cyclophosphamide 1.5g/m2/d×2 days and melphalan 110mg/m2/d×1 day. Two patients with T-LBL received BCNU+Etoposide+Cytarabine+Melphalan (BEAM) regimen. Graft-versus-host disease (GVHD) prophylaxis contained methotrexate (MTX), cyclosporine A (CsA) and mycophenolate mofetil (MMF), plus ATG (Rabbit anti-human thymocyte immunoglobulin, Sangstat) 1.5mg/kg/d iv daily from day -4 to -1 and additional 1.5mg/kg on day +7 (total dose of 7.5 mg/kg). In addition, anti-CD25 monoclonal antibody (basiliximab) 20 mg on day+1 and +4 was given iv. Donors were primed with G-CSF at 3-4 ug/kg/d sq d1-5. On day 4 of G-CSF, donor BM cells were harvested and were infused unmanipulated on the same day to patient on transplant day 01. On day 5 of G-CSF injection, donor primed PBMNCs were harvested, part of which were immediately infused unmanipulated to recipient on transplant day 02. Part of the cells were cryopreserved and stored in the liquid nitrogen, which were then thawed and reinfused unmanipulated to recipient on day +6 (Table 1).
Results
All patients achieved a trilineage engraftment with a median time of 13.5 (5-16) days. The median neutrophil and platelet engraftment were 13 (11-19) days and 10 (5-22) days respectively (Fig.1). Among 29 evaluable patients, acute GVHD occurred in 10 (34.5%, Fig. 2) with a median time of 32 (14-60) days, including 5 cases (17%) of grade Ⅱ, 3 (10%) of grade Ⅲ and 2 (7%) of grade Ⅳ. Among the 28 evaluable patients for chronic GVHD, only 6 (21.4%, Fig.3) developed limited chronic GVHD with a median time of 103 (90-180) days. Twenty seven out of thirty (90%) patients achieved disease-free survival (DFS) with a median follow-up time of 6 (5-14) months. Three patients died from transplant related complication, including infection for 2 and GVHD for 1 respectively.
Conclusion
In this study, with an intensive myeloablative condition and salvage haplo-HSCT, by reinfusing additional unmanipulated donor PBMNCs to recipients on day +6 during their transplantation, a short engraftment time without engraftment failure, low lethal GVHD incidence, and a lower infection rate were able to be achieved. More importantly, most patients remain DFS at a median follow-up time of 6 months. Despite short-term follow-up. the outcomes are particularly encouraging.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal