Introduction
Long-term hematopoietic stem cell transplant (HCT) survivors are burdened by a high prevalence and early onset of chronic diseases. Healthy dietary patterns have been associated with lower risks of chronic health conditions in the general population, yet no study to date has comprehensively documented the adherence of HCT survivors to the Dietary Guidelines for Americans (DGA), specifically designed to provide guidance for making healthy food choices. The aims of this study were to evaluate the extent to which HCT survivors adhere to the DGA and to determine nutrient intake adequacy. A secondary aim was to assess their willingness to take part in a future nutritional program or dietary intervention.
Methods
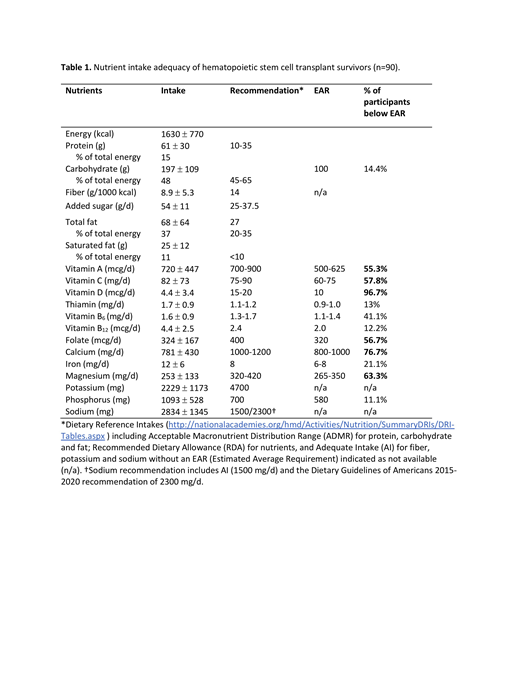
The study population included adults (≥18 y), who had undergone autologous or allogeneic HCT for a hematologic disease and were at least 1-year post-transplantation. Dietary intake was assessed using the Block 2014 food frequency questionnaire and diet quality (adherence to the DGA) was estimated using the Healthy Eating Index-2015 (HEI-2015). A HEI score of ≤50 indicates "poor diet quality", 51-80 suggests a "diet that needs improvement", and >81 indicates "good diet quality" out of maximum of 100. HEI-2015 scores by patient and transplant characteristics were analyzed by ANCOVA. Nutrient intake adequacies of the group were estimated by determining the percentage of the group falling below the Estimated Average Requirement (EAR) of the Dietary Reference Intakes. Receptivity to participate in a dietary intervention to stay healthy was measured by the question, "How willing would you be to take part in a healthy nutrition program or diet intervention?" Response categories included, "not at all," "somewhat," and "definitely".
Results
Between December 2017 and September 2018, 124 survivors were invited to participate, of whom 90 (51 autologous and 39 allogeneic HCT survivors) completed the dietary intake assessment and were included in the analysis. Majority were male (56%), White (72%), married (81%) and completed some college education (57%). Most participants were overweight (34%) or obese (37%). The median time from the HCT was 5.2 years. Mean ±SE HEI-2015 scores were 61.6 ± 1.3 and 60.7 ± 2.2 for the 18-64 y and ≥65 y age groups, respectively, slightly higher than the US general population. Adherence to a good quality diet was reported by only 10% of survivors. The majority of the survivors reported a diet in need of improvement (82%) or a poor-quality diet (8%). Intakes of vitamin A (720 ± 447 mcg/d), vitamin C (82 ± 73 mg/d), vitamin D (4.4 ± 3.4 mcg/d), magnesium (253 ± 133 mg/d), and calcium (781 ± 430 mg/d) suggested inadequacy, as more than 50% of the group fell below the specific EARs. Sodium intake at 2834 ± 1345 mg/d exceeded the DGA recommendation of 2300 mg/d. Fiber intake at 8.9 g per 1000 kcal/d was significantly below the Adequate Intake of 14 g per 1000 kcal/d. "Change in taste" was the only variable associated with lower quality of diet (p=0.02). Interestingly, 29% of HCT survivors reported persistent altered taste sensation. No significant relationships were seen for participant's demographics and diet quality which may be due to a sample population skewed toward older, causations and socioeconomically advantaged individuals. More than two thirds of participants (73%) indicated an interest in participating in dietary intervention. HCT survivors within 2 years of transplant were more likely to be receptive to participation in a diet intervention study compared to survivors beyond 2 years (52% vs 28%, p=0.0013).
Conclusion
Adult HCT survivors report poor adherence to the 2015 Dietary Guidelines for Americans and have numerous short-fall nutrient intakes. However, the willingness to participate in a nutritional program or dietary intervention in this survivorship population was relatively high. These findings reinforce the need to incorporate nutrition into HCT survivor care.
Wingard:Celgene: Consultancy; Merck: Consultancy; Shire: Consultancy; Ansun: Consultancy; Pluristem: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal