Introduction.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) could be curative for acute myeloid leukemia (AML) patients. However, the disease relapse after allo-HSCT lead to poor outcomes almost in all cases. Minimal residual disease (MRD) is a strong prognostic marker of increased risk of relapse and reflects overall (OS) and relapse-free survival (RFS) in patients with AML. Immunophenotypic evaluation using multiparameter flow cytometry (MFC) is an important strategy for detecting MRD, because of its simplicity and wide availability.
Aim. Determine the impact of MRD detected by MFC before allo-HSCT on clinical outcomes.
Patients and methods.
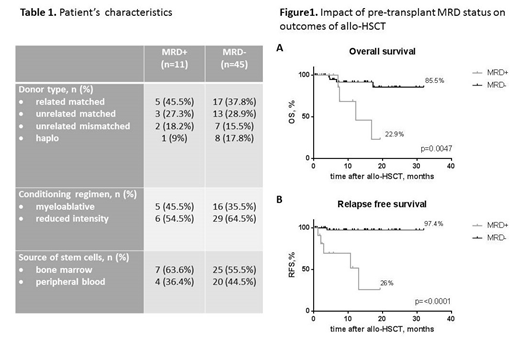
To assess the impact of MRD status before transplantation we include 56 AML patients who underwent allo-HSCT in National Research Center for Hematology between July 2016 and June 2019. Patient's characteristics are shown in table 1. All these patients were in first compete morphologic remission at the time of allo-HSCT. MRD was evaluated by MFC. Bone marrow samples were obtained before allo-HSCT and were analyzed by 6-color MFC (BD FACS Canto II, USA). Positive MRD was identified as a cell population deviating from the normal patterns of antigen expression on specific cell lineages at specific stages of maturation for all patients. In addition, for patients with LAIP at diagnosis, positive MRD was also defined as a cell population carrying LAIP markers at diagnosis.
The probabilities of OS and RFS were estimated using the Kaplan-Meier method.
Results.
Among 56 AML patients before allo-HSCT (all were in CR at the time of MRD analysis). Median of follow-up was 9.3 months.11 patients (19,6%) were identified as MRD+ (0,011%-5,08%, mean 1%). And 5 of them relapsed (45,5%). Out of 45 MRD negative patients before HSCT relapse was registered in one (relapse rate 2,2%). Statistical analysis revealed significant differences between MRD- and MRD+ patients: MRD+ had much worse OS (22,9% vs. 85.5%, p=0.0047, Fig.1A) and RFS (26% vs. 97.4%, p<0,0001, Fig.1B).
Conclusions.
Despite the presence of morphological CR before allo-HSCT, MRD persistence can lead to worse probabilities of OS and RFS, which is comparable to patients who were transplanted in relapse. Because of the association between MRD and relapse risk, it can be assumed, that testing for MRD before allo-HSCT may help to identify a subgroup of patients at high risk of relapse who might benefit from preemptive posttransplantation treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal