Introduction: Recent advances in next-generation sequencing (NGS) enables us to reveal the clinical relevance of age-related clonal hematopoiesis (ARCH) in healthy individuals without having hematologic disorders. It is plausible that transfer of ARCH from a donor to the recipient following allogeneic hematopoietic stem cell transplantation (HCT) results in delayed engraftment, thus increasing the risk of non-relapse mortality (NRM). A recent study reported that the presence of ARCH in the donor is associated with increasing risk of chronic graft-versus-host disease (GVHD) and reduced risk of relapse after allogeneic HCT (JCO 2018). However, detailed analyses are lacking with respect to engraftment, the severity of GVHD, organ-specific GVHD. The present study aimed to assess the impact of donor ARCH on HCT outcomes regarding overall and each organ-specific acute/chronic GVHD as well as engraftment kinetics.
Methods and patients: The present study includes 372 pairs of donors and/or recipients who received HCT from 2000 till 2007. Genomic DNA samples were archived from the samples taken prior to HCT. For barcoded error-corrected sequencing, a molecular inversion probe capture protocol was modified and applied (Gen. Research 2013). In short, we designed probes targeting 33 genes covering ARCH mutations along with other AML related mutations. Barcoded NGS library was generated and processed. Following sequencing (NovaSeq, Illumina) with 150 bp pair-end mode, the analysis was performed using a customized computational pipeline. Recipients and transplant characteristics are as following: male/female (n=223/149); median age, 48 yrs; conditioning regimen, reduced-intensity conditioning (RIC, n=105)/myeloablative conditioning (MAC; n=267). Median age of donors was 48 yrs. Transplant outcomes were analyzed according to the presence of ARCH in the donor in terms of overall survival (OS), NRM, relapse incidence (RI), overall acute and chronic GVHD as well as organ-specific incidences of GVHD. Engraftment parameters such as neutrophil and platelet recovery were also analyzed.
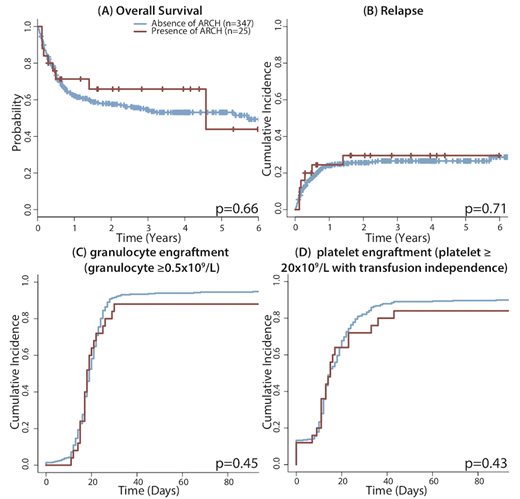
Results: 30 mutations were detected in 25 donor samples (6.7%). Consistent with previous studies, the most frequently mutated gene was DNMT3A (n=10/25, 40%). The median variant allele frequency (VAF) for 30 mutations in donor was 1.18% (ranges, 0.57%-13.29%). With respect to the presence or absence of ARCH in donors, there were no significant differences in baseline and transplant characteristics such as age, sex, conditioning regimen (RIC vs MAC), GVHD prophylaxis. The presence of ARCH in donor also did not show any difference in OS (p=0.66, HR 0.86 [0.44-1.68]), RI (p=0.71, HR 0.83 [0.31-2.21]) or NRM (p=0.7, HR 1.16 [0.54-2.51]).
With respect to the engraftment, the median time to neutrophil (defined as ≥0.5x109/L) and platelet engraftment (≥20x109/L with transfusion independence) was not associated with the presence of donor ARCH. Neutrophil engraftment rate was 88.0% in ARCH and 91.6% in the non-ARCH group at day 30 with a median time of 18 days and 19 days (p=0.45). The median time to platelet engraftment was 15 days both in ARCH and in the non-ARCH group (p=0.43).
In terms of GVHD, donor ARCH status did not affect incidences of aGVHD/cGVHD. Incidence of grade II to IV acute GVHD at day 100 was 69.9% and 66.2% in the ARCH and non-ARCH group (p=0.94). There were no differences between the two groups in organ-specific aGVHD of the skin (p=0.23), liver (p=0.98) or gut involvement (p=0.48). The cumulative incidence of chronic GVHD (based on the NIH consensus criteria) was 58.3% in ARCH and 58.6% in the non-ARCH group (p=0.80). No differences were noted in the severity of cGVHD between the 2 groups (p=0.87). No differences in organ-specific cGVHD were also noted for the ocular, oral, skin, liver, GI, lung or musculoskeletal involvement. Multivariate analyses confirmed that the donor ARCH was not significantly associated with survival, a/cGVHD and, engraftment after allogeneic HCT.
Conclusion: The presence of ARCH in the donor does not affect the mortality, relapse or engraftment following allogeneic HCT. Our data suggest that donor ARCH has no apparent association with HCT outcomes, although there was a concern on the presence of ARCH in the donor's HSCs and its transfer through allogeneic HCT. It also does not seem to delay engraftment or increase the risk of non-relapse mortality following allogeneic HCT.
Michelis:CSL Behring: Other: Financial Support. Mattsson:Gilead: Honoraria; Therakos: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal