Introduction:
Poor graft function (PGF) post allogeneic transplantation is defined as peripheral blood cytopenias in the presence of donor chimerism and is increasingly recognised as a specific clinical entity. The criteria for PGF diagnosis are variable with regards to level of donor chimerism level and duration of cytopenias. Patients with this condition are at high risk of complications from bone marrow failure and need to be differentiated from patients with persisting cytopenias that spontaneously recover without serious complications. We retrospectively analysed patients treated at our centre with complete donor chimerism and cytopenias in order to identify markers of poor prognosis and define an at-risk group that will form the basis of further clinical studies.
Method:
Patients who underwent allogenic stem cell transplant (alloHSCT) at our centre between 2000-2016 were included in this retrospective analysis after fulfilling the criteria for PGF (1) cytopenias in at least 2 lineages (defined as platelets <100x109/L, neutrophils <1.0x109/L, haemoglobin <100g/L)sustained for 30 days and (2) myeloid chimerism >95%. Patients with relapse of their haematological malignancy within 100 days post-alloSCT were excluded. The primary outcome variables were overall survival (OS) and death from PGF. OS was evaluated in landmark analyses from day 100 (D100) post-alloSCT. Variables were investigated for associations with OS using cox proportional hazards models. Relapse and death without PGF were treated as competing risks for the outcome of death from PGF; associations with PGF were investigated using the method of Fine and Gray. Variables statistically significant at α<0.05 were included in a forward step-wise fashion in multivariate models. Previous studies have demonstrated an excess of early mortality from PGF and hence patients were censored if alive at 24 months.
Results:
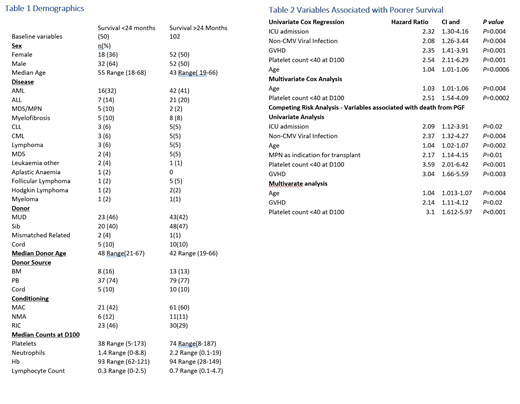
Of 908 transplants performed between 2000-2016, 152 patients (16%) fulfilled our criteria for PGF and were alive at day 100 post transplantation. The overall survival of the PGF cohort at 24 months was 65%. There were 102 patients alive at 24 months vs 50 who died within the 24 months period. The early mortality group had a median survival of 6 months (Range 3.3-23). Demographic details of the early mortality vs those who survived to 24 months are listed in Table 1. Univariate analysis of the PGF cohort identified the following variables were significantly associated with inferior OS: non-CMV viral infection, ICU admission during initial 30 days, age as a continuous variable, grade 2-4 acute GVHD and platelet count ≤40x109 /L (P40) at D100. Age and P40 remained significantly associated with OS on multivariate analysis. Hazard ratios and P values are summarised in Table 2.
Competing risk analysis revealed, Age, non-CMV viral infections, ICU admission, MPN as an indication for transplantation, P40 at D100 and grade 2-4 GVHD as significant associations for death from PGF.
Age, GVHD and P40 remained significantly associated with death from PGF in multivariate analysis. Hazard ratios and P values are summarised in Table 2.
Conclusion:
Increasing patient age and marked thrombocytopenia at D100 are associated with inferior survival in patients with PGF. These factors identify patients at higher risk of death from PGF which inform a stricter definition of the syndrome and provide a population for future interventional studies.
Ritchie:Sanofi: Honoraria; Novartis: Honoraria; Imago: Research Funding; Beigene: Research Funding; Takeda: Research Funding; BMS: Research Funding; Pfizer: Consultancy; Amgen: Consultancy, Honoraria, Research Funding. Koldej:NanoString Technologies: Other: Travel grant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal