Introduction:
Hematopoietic stem cell transplantation (HSCT) is associated with severe intestinal microbiota injury as a consequence of broad spectrum antibiotics, mucosal damage from conditioning, and dietary changes. Intestinal dysbiosis has been correlated with adverse outcomes post-transplant. We aimed to characterize and compare the patterns of microbiota injury that occur post autologous and allogeneic transplant. We characterized the specific risk factors associated with decreased microbial diversity in HSCT, and defined specific bacterial taxa that are enriched or depleted in patients based on the type of transplant and various other risk factors
Methods:
Stool samples from 35 patients (pts) undergoing HSCT were collected immediately pre-conditioning, at day 14, 28, and 100 post-transplant. 17 pts underwent an autologous (auto-) and 18 pts underwent an allogeneic transplant (allo-HSCT). The stool microbiome was characterized by sequencing of the V3V4 16s rRNA region; a- and b-diversity were determined and differential abundance analysis of OTUs was performed using DESeq2.
Results:
In the auto-HSCT cohort 70% of pts had plasma cell dyscrasia, and 24% had non-Hodgkin lymphoma. 83% of pts in the allo-HSCT cohort had a myeloid neoplasm, and 17% had a T cell neoplasm. 33% of pts undergoing allo-HSCT developed grade 2-4 GVHD within 100 days and 56% developed GVHD within 6 months.
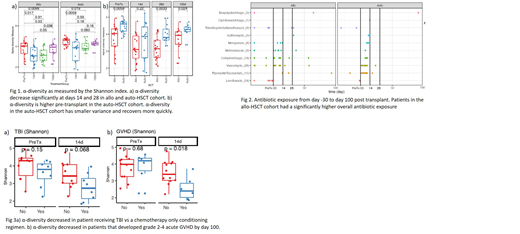
The pre-transplant intestinal microbiome α-diversity was significantly higher in pts undergoing auto-HSCT compared to allo-HSCT (Fig 1). The etiology for this was likely multifactorial. More pts in the allo-HSCT cohort had received antibiotics within 30 days prior to transplant, compared to the auto-HSCT cohort (56% vs 18%). Pts in the allo-HSCT cohort had a higher proportion of VRE or MDR Gram-negative bacteria on screening cultures (44% vs 29%), which may be associated with domination of certain species.
In both the allo- and auto-HSCT cohorts, the α-diversity significantly decreased at days 14 and 28, but recovered to pre-transplant levels by day 100. Pts in the auto-HSCT cohort displayed faster recovery kinetics, and had a significantly higher α-diversity at day 28 compared to the allo-HSCT cohort (Fig 1). The microbiome recovery in the auto-HSCT cohort was consistent across the whole group and was characterized by a much smaller variance compared to the allo-HSCT cohort. This may reflect lower total antibiotic exposure in the auto-HSCT cohort (Fig 2). Other factors specific to the allo-HSCT cohort were the occurrence of GVHD and the use of TBI, both of which were associated with decrease in α-diversity in our population (Fig 3).
Of note, Faecalibacterium prausnitzii was found to have a >20 log reduction in both the auto and allo-HSCT cohorts. It is a commensal gut bacterium, and its depletion has previously been reported in inflammatory bowel disease. There is very limited data on this bacterium in the peri-transplant setting. It has an anti-inflammatory effect on the intestinal microenvironment through production of butyrate, inhibition of NF-kB, upregulation of regulatory T cell production, and release of metabolites that enhance intestinal barrier function (Lopez-Siles et al, ISME 2017). Transplantation of F. prausnitzii has been shown to decrease inflammation in mice models of colitis (Sokol 2009).
We then evaluated the association between microbiota injury and GVHD. α-diversity was significantly decreased at day 14 and day 28 in pts who developed GVHD within 100 days. In differential abundance analysis of samples from pts who developed acute GVHD within 6 months, there was a >20 log reduction in the Bifidobacterium, Blautia, and Eubacterium Dolichum. Decrease in Blautia has previously been associated with increased GVHD related mortality. Bifidobacterium and Eubacterium Dolichum have not been reported in association with GVHD in humans before. All three bacterial taxa reported here are involved in production of short chain fatty acids, which may provide a common protective mechanism.
In summary, this study showed that pts undergoing autologous transplant have a healthier pre-transplant microbial diversity, and that microbiota injury heals quicker after transplant. We have identified TBI as a risk factor for microbiome injury, which has not been previously studied in the context of HSCT. We also identify previously unreported bacterial taxa whose depletion is strongly associated with GVHD.
Assal:Incyte corporation: Consultancy, Research Funding; boston biomedical: Consultancy. Uhlemann:Merk: Research Funding; GSK: Research Funding; Allergan: Research Funding. Reshef:Kite, a Gilead Company: Consultancy, Honoraria, Research Funding; Atara: Consultancy, Research Funding; Magenta: Consultancy; Pfizer: Consultancy; Pharmacyclics: Consultancy, Research Funding; Celgene: Research Funding; Incyte: Consultancy, Research Funding; Shire: Research Funding; BMS: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal