Background. Reduced-intensity conditioning (RIC) regimens are commonly used for hematopoietic cell transplantation (HCT) in non-malignant disorders to minimize potential drug-related toxicity from myeloablative conditioning (MAC). However, melphalan-based RIC regimens are associated with poor engraftment and need for second HCT or donor lymphocyte infusions (DLIs). This study expands on our previous experience with targeted busulfan, fludarabine, and intravenous (IV) alemtuzumab as a low-toxicity but myeloablative regimen to achieve sustained donor engraftment.
Methods. We conducted a retrospective analysis of patients ≤25 years of age with non-malignant disorders who received targeted busulfan, fludarabine and IV alemtuzumab as conditioning for their first HCT between 2004 and 2018. Graft-versus-host disease (GVHD) prophylaxis included calcineurin inhibitors in all patients, plus methotrexate (n=59), methylprednisolone (n=2), or mycophenolate (n=1). The primary end point was 3-year overall survival (OS). Secondary end points included treatment-related mortality (TRM), event-free survival (EFS) defined as alive without second HCT or disease progression, and incidence of acute and chronic GVHD (aGVHD and cGVHD). Other end points included incidence of graft failure (GF) defined as <5% donor chimerism in whole blood, sinusoidal obstruction syndrome (SOS) and CMV viremia. Analysis was stratified by era of HCT (2004-2011 vs. 2012-2018).
Results. We identified 62 patients with a median age of 5.5 years and male:female of 46:16. Diagnoses included primary immune deficiencies (60%), hemoglobinopathies (22%), bone marrow failure disorders (8%) and inherited metabolic disorders (10%). The median busulfan cumulative area-under-the-curve (cAUC) was 70 mg*h/L (range, 57-108 mg*h/L). Donors were matched sibling (MSD) in 27%, 8/8 allele-matched unrelated (MUD) in 50% and Class I allele-mismatched (MM) in 23%. All but 2 of the Class I allele-MM donors were unrelated. The source was bone marrow (BM) in 74% and peripheral blood stem cells (PBSC) in 26%.
The cumulative incidence (CI) of GF was 8% (95% CI, 1-16%). In engrafted patients, the median donor chimerism in whole blood, CD3, CD14/15, and CD19 at 1-year was 96%, 90%, 99%, and 99%, respectively. Only 1 patient required DLIs for poor chimerism. T-cell reconstitution (CD4 >200 x 109/L and PHA response >50% control) was achieved at a median of 182 days (range, 76-585 days). Two patients died following disease progression despite 100% donor chimerism.
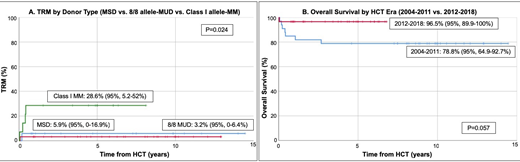
The CI of TRM was 10% (95% CI, 2-17%). Causes of TRM included infectious complications (n=2), hemorrhage (n=1), respiratory failure (n=3 with 2 following subsequent transplants after graft rejection). TRM incidence was significantly higher in patients with Class I MM compared to those with MSD or 8/8 allele-MUD (29% vs 6% vs 3%; p=0.024; Figure 1A). SOS occurred in 5% of patients and all resolved with supportive therapy (n=1) or defibrotide (n=2). Post-transplant CMV viremia occurred in 26% of all patients and in 71% of CMV seropositive patients. None developed CMV disease and all infections resolved with anti-viral therapy.
OS and EFS at 3-years were 87% (95% CI, 78-95%) and 80% (95% CI, 70-90%), respectively. HCTs performed in the more recent era showed an OS of 97% compared to 79% in HCTs performed earlier (p=0.057; Figure 1B). OS was 97% in patients with 8/8 allele-MUD compared to 79% in those with MSD and 71% in those with Class I allele-MM (p=0.051). The 6-month CI of grade II-IV aGVHD was 7% (95% CI, 3-13%), while the 3-year CI of cGVHD was 5% (95% CI, 0-11%). GVHD incidence was higher in patients receiving PBSC compared to BM (25% vs 0%; p<0.001) and in patients ≥5 years of age compared to those <5 years of age (13% vs 0%; p=0.043). Patients with inherited metabolic disorders showed significantly worse OS (44%, p=0.016), EFS (33%, p=0.001) and aGVHD (33%, p=0.008) than those in other disease groups. Univariate analysis did not show any significant differences in survival or GVHD incidence by race or sex.
Conclusions.
Use of targeted busulfan, fludarabine and IV alemtuzumab as myeloablative conditioning in pediatric patients with primary immunodeficiencies, hemoglobinopathies, and bone marrow failure syndromes undergoing matched sibling or well-matched unrelated donor HCT provides a well-tolerated option to achieve sustained engraftment with low incidence of GVHD and toxicities such as SOS.
Shimano:Pfizer: Research Funding; Daiichi Sankyo: Research Funding; Novartis: Research Funding. Huang:Novartis: Research Funding. Cowan:Homology Medicine: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Leadiant: Consultancy; California Institute Of Regenerative Medicine: Research Funding; NIH NIAD: Research Funding; Rocket Pharma: Consultancy; UpToDate: Honoraria; bluebird bio: Consultancy. Dvorak:Alexion Inc: Consultancy; Jazz Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal