Background: Several population-based studies on multiple myeloma (MM) have shown an improvement in relative survival (RS) for patients aged 65 years or younger at the time of diagnosis. In patients aged 75 years or older, the improvement in long-term RS is absent in most reports or much less pronounced. To our knowledge, only 2 studies based on the Surveillance, Epidemiology and End Results (SEER) database have demonstrated a significant increase in RS for this age-group. (Pulte et al. 2011, Costa et al. 2017) We performed a population-based study on Norwegian MM-patients to provide up-to-date estimates on changes in relative survival during the past 3 decades.
Methods: The Cancer Registry of Norway (CRN) was established in 1951 and provides high-quality nationwide cancer statistics. For MM, the reported completeness of case-ascertainment is above 95%. Incidence data and all reported cases of MM diagnosed between January 1, 1982 and December 31, 2017 were retrieved from the CRN (n=10 961). Nationwide drug consumption statistics for drugs used in myeloma treatment were retrieved from the Norwegian Drug Wholesales Statistics and the Norwegian Prescriptions Database, Norwegian Institute of Public Health. Follow-up ended December 31, 2017. The time of MM-diagnosis was divided into 7 categories: 1982-1987, 1988-1992 (melphalan-prednisone), 1993-1997(early high-dose melphalan with autologous stem-cell transplant (HDM-ASCT)), 1998-2002 (introduction of thalidomide), 2003-2007 (early thalidomide upfront, introduction of bortezomib), 2008-2012 (thalidomide and bortezomib upfront, introduction of lenalidomide), 2013-2017 (lenalidomide upfront, early pomalidomide, daratumumab, panobinostat and carfilzomib). Age at diagnosis was divided into 3 categories; <65 years, 65-79 years and 80 years or older. We estimated relative survival ratios (RSR) with 95% confidence intervals 5 and 10 years after the time of diagnosis by the Ederer-II method. The analysis was stratified by age-group and calendar period of diagnosis. Cohort analysis was applied to calendar periods with complete follow-up, and period analysis was applied where complete-follow up was not available (2013-2017 and 10-year estimates for 2008-2012). Non-overlapping confidence intervals were considered statistically significant.
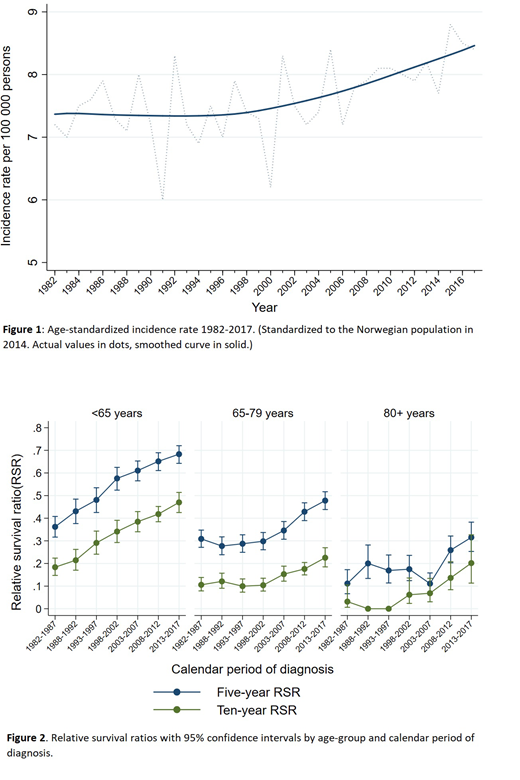
Results: The age-standardized incidence rate was stable until approximately year 2000, followed by an increasing tendency reaching 8.4 cases per 100 000 persons in 2017. Figure 1. Patients diagnosed before the age of 65 had a steady increase in both 5 and 10-year RSR across all calendar periods. For patients aged 65-79 years, the 5- and 10-year RSR's were stable at approximately 0.3 and 0.1, respectively, until the calendar period 1998-2002. In the following years, an improvement in both 5- and 10-year RSR was observed. The 5-year RSR improved significantly from 0.31 (95% CI; 0.27-0.35) in the first calendar period to 0.43 (95% CI;0.39- 0.47) during 2008-2012. The predicted 5-year RSR for 2013-2017 was 0.48 (95% CI; 0.44-0.52). There were also signs of improved 10-year RSR, predicted to 0.23 (95% CI; 0.18-0.27) during 2013-2017 compared to 0.11 (95% CI; 0.08-0.14) during 1982-1987. The 5-year RSR for patients aged 80+ years was 0.11 (95% CI; 0.01-0.17) during 1982-1987 and the 10-year RSR was 0.03 (95% CI; 0.01-0.11). In the following 4 calendar periods the RSR-estimates fluctuated before a rising tendency during the last 2 periods. The 5-year RSR improved significantly to 0.26 (95% CI; 0.20-0.32) during 2008-2012 and further rising to a predicted value of 0.32 (95% CI; 0.25-0.38) during 2013-2017. Figure 2. Additionally, complete annual prescription statistics for the oral agents thalidomide, lenalidomide and pomalidomide were obtained.
Conclusions: We provide real-world observations on changes in RS in a population-based cohort of 10 961 MM-patients. We demonstrate an improvement in 5-year relative survival across all age-groups, including patients aged 80 years or older. For patients <65 years, there was a steady increase in RS since 1982 and we see no obvious impact of the implementation of HDM-ASCT. For the other age-groups, the improvement in RS coincides with the introduction of new drugs. The increase in incidence since 2000 may be due to increased testing for M-protein. We can point to the introduction of new drugs and increased incidence of indolent cases as possible reasons for increasing RS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal