Background: Suppression of uninvolved immunoglobulins [Ig], or immunoparesis, is associated with an inferior progression-free survival [PFS] and overall survival [OS] in patients with newly diagnosed multiple myeloma [MM]. However, immunoparesis in relapsed MM can be either due to the underlying disease or prior anti-myeloma therapy or both. Data on characterization and prognostic impact of immunoparesis in relapsed MM is lacking in the era of proteasome inhibitors and immunomodulatory drugs. We hypothesized that immunoparesis in relapsed MM is a marker of high tumor burden or adverse biology and is associated with an inferior post-relapse survival.
Method: We evaluated all MM patients diagnosed between 1/1/2008 and 12/31/2015 at the Cleveland Clinic and followed until 05/31/2019. Key inclusion criteria were patients experiencing first relapse requiring an additional line of therapy and available data on pre-therapy immunoglobulin levels. Both Qualitative and Quantitative immunoparesis were defined using the method described earlier [Muchtar et al. Leukemia. (2017) 31. 92-99]. Qualitative immunoparesis was categorized as No [preserved uninvolved Igs], Partial [suppression of at least one but not all uninvolved Igs], or Full [suppression of all uninvolved Igs]. For quantitative immunoparesis, the average relative difference [ARD] from the corresponding lower limit of normal was calculated. Recursive partitioning analysis was performed with a log-rank splitting method to identify an optimal ARD cut-point for OS. The primary endpoints were PFS and OS from first relapse, which were estimated using Kaplan-Meier method and groups were compared with log-rank test. Cox proportional hazards analysis was used to identify univariable and multivariable prognostic factors for PFS and OS.
Results: A total of 527 patients with newly diagnosed MM were evaluated, among which, 258 [49%] experienced first relapse and formed the study cohort. The median age at first relapse was 64 years, with a median of 24.5 months from diagnosis to first relapse. Front-line therapy included bortezomib in 77% and lenalidomide in 76% of patients. A total of 217 [85%] patients relapsed on therapy, the most common being maintenance with PI or IMiD [+/- steroid]. Biochemical-only relapse happened in 56% of patients.
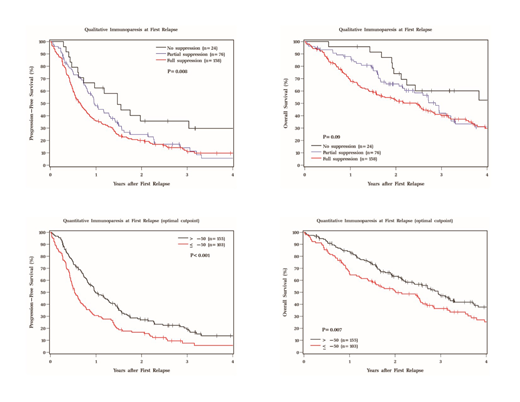
The distribution of qualitative immunoparesis at first relapse was: No [n=24; 9%], Partial [n=76; 30%], or Full [n=158; 61%]. For quantitative immunoparesis, the median ARD was -39% [range, -92 to 241], with higher negative values indicating deeper immunoparesis. The median ARD was +67%, +15%, and -58% in No, Partial, Full immunoparesis subgroups respectively [P<0.001]. At a median follow-up of 34 months from first relapse, 2-year PFS in No, Partial, and Full immunoparesis subgroup was 36%, 25%, and 20% respectively [P=0.008]. The 3-year OS in respective subgroups was 60%, 42%, and 40% [P=0.09]. For quantitative immunoparesis, the optimal ARD cut-point for OS was -47%, which was rounded to -50% for ease of interpretation. Hence, patients were divided into 2 groups: >-50% [n=155; 60%] and ≤-50% [n=103; 40%]. Higher immunoparesis depth [ARD≤-50%] at first relapse was significantly associated with the following: abnormal karyotype at diagnosis, deeper immunoparesis at diagnosis, less than a very good partial response [VGPR] in first remission, ≤12 months from diagnosis to first relapse, high serum free light chain ratio, β-2 microglobulin, and lactate dehydrogenase at first relapse, and low hemoglobin at first relapse. Notably, relapse on therapy versus on observation was not associated with the depth of immunoparesis at first relapse. The 2-year PFS in >-50% and ≤-50% subgroup was 27% and 17% respectively [P<0.001], with respective 3-year OS of 47% and 36% [P=0.007]. In multivariable analysis [MVA] assessing qualitative immunoparesis, immunoparesis remained prognostic for PFS but not OS. In MVA assessing quantitative immunoparesis, it remained prognostic for both PFS and OS. The Kaplan-Meier curves for PFS and OS with qualitative and quantitative immunoparesis are shown in Figure I.
Conclusion: Depth of immunoparesis at first relapse is an additional prognostic factor for post-relapse survival in MM in the era of novel agents and continuous therapy. The clinical implication of immunoparesis as a prognostic factor is further amplified by the widespread availability of immunoglobulin measurement.
Valent:Amgen corporation: Speakers Bureau; Celgene corporation: Speakers Bureau; Takeda pharmaceuticals: Speakers Bureau. Anwer:Seattle Genetics: Membership on an entity's Board of Directors or advisory committees; In-Cyte: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal