Sickle cell disease (SCD) is the most common genetic condition in the world and disproportionately affects African Americans in families with lower household incomes. SCD is characterized by a variety of complications including episodes of severe pain, chronic anemia, and end-organ damage. Morbidity from SCD begins in infancy and increases in frequency and severity with age. Complications during childhood and adolescence, both critical learning periods for youth, substantially impact educational attainment and life outcomes.
SCD-related hospitalizations are associated with social determinants of health, such as socioeconomic status (SES), depression, health literacy, and educational outcomes. In youth with SCD, family and neighborhood SES are predictors of pain level, pain frequency, and overall quality of life. In addition to the physiological impacts of SCD, individuals with SCD experience emotional and stress related effects of the disease that may impact daily quality of life and frequency and severity of pain. Studies have found that hospital admission frequency has limited or no impact on academic outcomes in youth with SCD. Few studies have explicitly examined the relationship between SCD-related pain and educational, socioeconomic, and mental health outcomes.
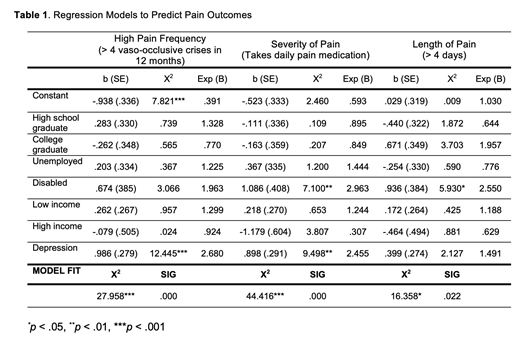
This is a cross-sectional study of patient survey data from a single site in the Sickle Cell Disease Implementation Science Consortium (SCDIC). The primary objective was to identify a relationship between educational attainment, employment status, mental health, and the frequency, severity, or length of pain crises for individuals with SCD. Multivariate analysis was used to assess the impact of patients' educational attainment, employment status, annual household income (low = less than $25,000, high = $75,001 and above), and self-reported depression on the frequency, length, and severity of SCD-related pain. Our central hypothesis was that individuals with a history of depression, lower educational attainment, periods of unemployment, and lower incomes experience more frequent, more severe, and longer pain crises.
A total of 307 participants were included. The mean age was 27.4 years (range 15 to 45), 58.3% were female, and 99% were African American. Sixty-two percent had Hgb SS, the most severe form of SCD. About half of all patients (50.5%) reported they take pain medication every day for SCD and majority were on some form of disease modification (64.2% on hydroxyurea (HU), 20.2% on chronic blood transfusion). Slightly less than half (48.9%) reported their highest level of education as a high school diploma or lower. Most were unemployed (15.3%), students (22.8%), or disabled (21.5%), and 59.2% reported an average annual household income less than $25,000. Univariate analysis revealed statistically significant associations between employment status as unemployed or disabled and frequency of pain (p < .001), employment status as unemployed or disabled and severity of pain (p < .001), and employment status as disabled and length of pain > 4 days. Relationships between depression and frequency and severity of pain were statistically significant at the p < .001 level, and between depression and length of pain > 1 week at the p < .01 level. Multivariate analysis revealed positive statistically significant relationships between depression and high pain frequency (p < .001), employment status as disabled and severe pain (p < .01), depression and severe pain (p < .01), and employment status as disabled and length of pain >4 days (p < .05), Table 1. Educational attainment did not demonstrate statistically significant relationships with pain outcomes. No variables demonstrated statistically significant relationships with length of pain > 1 week and length of pain > 2 weeks. The only significant association with pain outcomes was that HU users were less likely to take daily opioids.
Individuals with SCD who are disabled or have a history of depression are more likely to report more severe and frequent pain. No relationship emerged between educational attainment and pain outcomes. As the results are limited to the cross-sectional design, we cannot make statements of causality. For now, we know that people with SCD and these risk factors need further study for interventions. We plan to further assess study participants across all eight SCDIC sites in the next phase of this work.
King:Bioline: Consultancy; Amphivena Therapeutics: Research Funding; Incyte: Consultancy; Cell Works: Consultancy; Celgene: Consultancy; Magenta Therapeutics: Membership on an entity's Board of Directors or advisory committees; Novimmune: Research Funding; RiverVest: Consultancy; Tioma Therapeutics (formerly Vasculox, Inc.):: Consultancy; WUGEN: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal