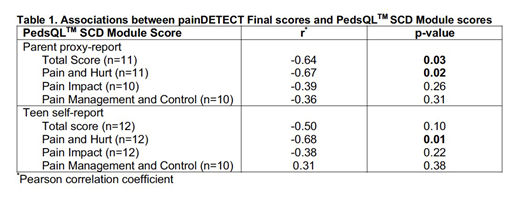
Background. The hallmark complication of sickle cell disease (SCD) is pain - both acute pain and chronic, daily pain that worsens with increasing age. Emerging data reveal patients with SCD display features of nervous system sensitization, with associated thermal and mechanical hypersensitivity and neuropathic pain. Children with SCD report impaired health-related quality of life (HRQL) when compared to healthy race-matched controls. In addition, more severe SCD is associated with worse HRQL. Further, data show approximately 40% of patients with SCD report neuropathic pain. The presence of neuropathic pain is associated with poor HRQL in non-SCD pain conditions, but this relationship in SCD is unknown. Thus, we sought to investigate associations between neuropathic pain and HRQL in adolescents with SCD. We hypothesized that neuropathic pain is associated with worse HRQL in adolescents with SCD. Methods. We conducted a cross-sectional study of patients with SCD ages 13-18 years presenting for a clinic visit. All patients were in their baseline state of health, defined as no emergency department visits or hospitalizations for a SCD-related complication, including acute pain crisis, for at least 7 days prior to the completion of either assessment. Primary outcome was HRQL, assessed by the PedsQLTM SCD Module (child self-report and parent proxy-report). Neuropathic pain was assessed using the painDETECT questionnaire. PedsQLTM SCD Module is a 43-item questionnaire that encompasses 9 scales: (1) Pain and Hurt, (2) Pain Impact, (3) Pain Management and Control, (4) Worry I, (5) Worry II, (6) Emotions, (7) Treatment, (8) Communication I and (9) Communication II. This study focused on the following: Total Score, Pain and Hurt, Pain Impact and Pain Management and Control scales. PedsQLTM SCD Module is scored resulting in a Total Score (0-100) and individual scale scores (0-100). Higher scores indicate better HRQL; scores from 0-60 indicate poor HRQL. The painDETECT questionnaire is a 12-item screening tool used to differentiate neuropathic from non-neuropathic pain, validated for use in ages ≥14 years. painDETECT is scored from 0-38; scores between 13 and 38 indicate a probable or definite component of neuropathic pain. Descriptive statistics were used to summarize patient demographic characteristics, PedsQLTM scores and painDETECT scores. Pearson correlation coefficients were used to examine the associations between painDETECT and PedsQLTM Total Score, Pain Impact, Pain and Hurt and Pain Management and Control Scores. Analyses for child self-report and parent proxy-report were performed separately. A p<0.05 was considered statistically significant. Results. Twelve patients were enrolled. The median (IQR) age was 15 (14-16.5) years, 75% were female and 83.3% were on hydroxyurea. All patients completed both PedsQLTM SCD Module and painDETECT questionnaire. Median PedsQLTM SCD Module child self-report Total Score was 51.75 (IQR 48.26-55.58) and 83.3% had a Total Score between 0-60. Median PedsQLTM SCD Module parent proxy-report Total Score was 54.49 (IQR 40.12-66.28) and 63.6% had a Total Score between 0-60. The median painDETECT score was 10.5 (IQR 4.5-14.5) and 41.7% had a painDETECT score of 13-38, indicating a probable or definite component of neuropathic pain. Higher painDETECT scores were significantly associated with lower PedsQLTM parent proxy-report Total Scores and Pain and Hurt Scores (Table 1). Higher painDETECT scores were also significantly associated with lower PedsQLTM SCD Module child self-report Pain and Hurt Scores (Table 1). There were no significant associations between painDETECT scores and Pain Impact or Pain Management and Control Scores (Table 1). Conclusions. Adolescents with SCD and neuropathic pain have worse HRQL, as reported by the child and the primary caregiver, even in their baseline state of health. These data provide preliminary evidence for a multimodal approach to pain assessment. Continued investigation of this relationship is warranted in order to further characterize the association between neuropathic pain and HRQL in patients with SCD over time.
Panepinto:NIH: Research Funding. Brandow:NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal