[Introduction]Modified Barthel Index (MBI) is widely used to measure performance in activities in daily living (ADL), especially in elderly patients. MBI consists of 10 items: feeding, personal hygiene (grooming), bathing, dressing, toilet transfer, bladder control, bowel control, chair/bed transfers, stair climbing, and ambulation. A total score ranges from 0 to 20. MBI has been studied in several types of cancer which is correlated with prognosis. However, the prognostic role of MBI in diffuse large B-cell lymphoma is still unknown. The study aims to investigate the predictive role of MBI in elderly patients over 60 years with DLBCL.
[Methods]This retrospective study included elderly DLBCL patients over 60 years treated at our institution between 2009 and 2018. MBI score of each patient was evaluated at diagnosis. Receiver operator characteristic (ROC) curve was used to generate a cut off value for MBI. Kaplan-Meier method and univariate, multivariate analysis by Cox proportional hazards model were performed to assess the prognostic influence of the factors including Stage, Revised International Prognostic Index score (R-IPI), Performance status (PS), Extra-nodal Site Involvement (ESI), Lactate Dehydrogenase (LDH), Soluble Interleukine-2Receptor (sIL-2R), Albumin, B symptoms and MBI. The study protocol was approved by the Institutional Review Board of Yokohama Municipal Citizen's Hospital, and it was carried out in accordance with the Declaration of Helsinki.
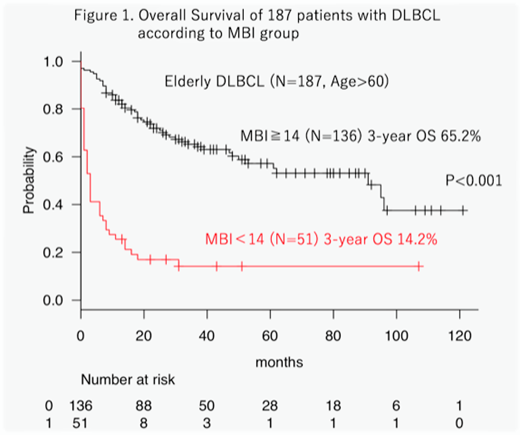
[Results]A total of 187 patients were included in the analysis. There were 102 males and 85 females, with a median age of 77 (range: 61-93). The median follow-up time was 39 months. The optimal MBI cutoff value for predicting 3-year survival was determined by ROC analysis to be 14.Patients with low MBI scores (< 14) had significantly shorter overall survival (OS) than those with high MBI scores (≥ 14) (3-year OS, 14.2 % vs. 65.2 %, p < 0.001). Among 163 patients receiving chemotherapy, patients with low MBI scores had shorter OS than those with high MBI scores (3-year OS, 21.2 % vs. 66.4 %, p < 0.001). In multivariate analysis, parameters having independent adverse significance for OS were: Low MBI (< 14) (p < 0.001, HR 2.49), PS ( ≥ 2) (p=0.04, HR 1.84).
[Conclusion]In the present study we demonstrated that Low MBI was deeply associated with poor outcome in elderly patients with DLBCL. In particular, our data proved that a low MBI is an independent prognostic factor for survival in elderly patients with DLBCL. These results suggest that Low MBI may have an important role in DLBCL and may be also a useful prognostic marker. Since our results are based on a small-sized analysis, further large prospective studies are warranted to verify this conclusion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal