Introduction:
Patients (pts) with CTCL have disruption in their skin barrier and are at increased risk for cutaneous infections. In particular, staphylococcal infections are common in pts with CTCL and are associated with pathogenesis of the lymphoma. Previous studies have identified extra-cutaneous involvement of lymphoma as the most important independent risk factor for recurrent skin infection, bacteremia, and death from infection. However, the risk of mortality with bacteremia and risk factors for developing bacteremia in CTCL have not been fully elucidated. We aimed to explore risk factors for bacteremia and subsequent mortality in pts with CTCL at Emory University.
Methods:
We conducted a single center retrospective analysis at the Winship Cancer Institute of Emory University analyzing CTCL pts from 01/01/1990 - 06/01/2019. We selected pts from an existing cutaneous lymphoma database and separated them by presence or absence of bacteremia at any point following diagnosis. Bacteremia was defined as identification of at least one microbe in the bloodstream on culture. The primary objective was to assess 90-day mortality among pts with CTCL with bacteremia. Secondary objectives included assessing patterns of care in bacteremic pts, identifying risk factors for bacteremia incidence and for poor outcomes following bacteremia (defined as a composite outcome of intensive care unit stay, mortality at 90 days, or re-current hospitalization within 90 days). Additionally, we explored patterns of oral antibiotic use in the outpatient setting and their association with bacteremia incidence and outcomes. Prophylactic skin antibiotics were defined in the notes as "prophylactic" i.e. not being used to treat active cellulitis or other infections. Categorical variables were analyzed with chi-squared tests.
Results:
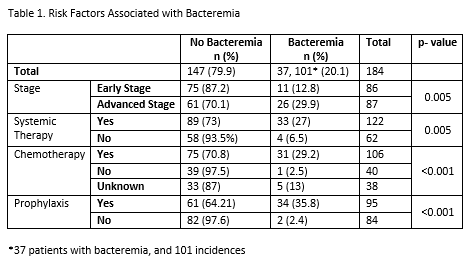
184 of 549 pts identified from our cutaneous lymphoma database were included in our analysis. Patients were excluded for lack of follow up or missing data. The median age was 57. Most pts had mycosis fungoides (n=137), followed by Sézary syndrome (n=20), CTCL, NOS (n=12), and CD30+ variants (n=6). 85 pts were early stage, and 87 were advanced stage (stage 2B n=41; 3 n=16; 4 n= 30) at diagnosis. 37 of 184 pts (20.1%) developed bacteremia. 95 pts used intermittent skin prophylactic antibiotics in the outpatient setting, 84 did not, and 5 were unknown. A total of 101 bacteremic episodes were noted (range of 1-10 per pt). The most common organisms were Staphylococcus species (sp) (MRSA n=21, MSSA n=10, other staph n=10). Other organisms included Corynebacterium sp., Enterococcus sp., Acinetobacter sp., Pseudomonas sp., and Escherichia-coli. Polymicrobial bacteremias were noted in 23 pts (28.8%). 42 (40%) had concurrent positive skin/wound . 69 pts (86.3%) were taking oral at the time of bacteremia. 71 pts were hospitalized for bacteremia (88.8%), and 41 pts (51.3%) had a recurrent admission within 90 days of discharge. 45 pts (56.3%) had invasive lines prior to bacteremia, and 44 of these had them removed following bacteremia. 71 (88.8%) cases were treated with appropriate antibiotic coverage. 56 pts were receiving active disease therapy at the time of bacteremia (70%), including 33 who were receiving systemic therapy. Intermittent prophylactic antibiotic use was highly associated with development of bacteremia (p < 0.001, table 1), as was advanced stage (12.8% early stage patients developed bacteremia compared to 29.9% of advanced stage, p=0.005). Prior systemic therapy, and in particular chemotherapy was associated with increased incidence of bacteremia (31 of 106 (29.2%) patients treated with chemotherapy developed bacteremia, p=0.0003) Extra-cutaneous disease was not associated with bacteremia in our analysis. The 90-day mortality among CTCL pts developing bacteremia was 11.25%.
Conclusions
This is the largest study assessing outcomes and risk factors for bacteremia in CTCL in the modern era. We confirmed that bacteremia is associated with high rates of re-admission, recurrent infection, and 90-day mortality, and identified advanced stage and use of chemotherapy as risk factors associated with bacteremia. The positive association of prophylactic antibiotics with bacteremia likely represents increased prescribing of skin prophylaxis among those at higher risk for bacteremia. Uni-variate, multivariate, and survival analyses will be updated at the time of the presentation.
Lechowicz:Kyowa: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal