Introduction: Marginal zone lymphoma (MZL) and lymphoplasmacytic lymphoma (LPL)/Waldenstrom's macroglobulinemia (WM) comprise approximately 7% and 2%, respectively, of non-Hodgkin's lymphomas (NHL) (Teras 2016). MZL is further subclassified as splenic MZL (sMZL), nodal MZL (nMZL), or extranodal MZL (eMZL). Standard first-line therapies for LPL/WM include rituximab plus an alkylating agent and/or proteasome inhibitor or ibrutinib (Castillo 2017), while standard first-line treatment for MZL varies by subtype (Rosand 2017). There are limited treatment options for patients who have relapsed after first-line therapy. Idelalisib, a selective oral inhibitor of PI3Kδ, demonstrated efficacy in indolent NHL (iNHL), including MZL and LPL/WM, at a median follow-up of 9.7 months (mos) in a phase 2 study (NCT01282424; 101-09; Gopal 2014). Here, we present the final, long-term results for patients with double-refractory MZL and LPL/WM from the 101-09 study.
Methods: Eligible iNHL patients had measurable disease and were refractory to both rituximab and an alkylating agent. Refractory status was defined as lack of response to or progression of lymphoma within 6 mos of completion of preceding therapy, documented by imaging. Oral idelalisib 150 mg twice daily was administered continuously until disease progression or intolerance. Responses were evaluated by an independent review committee using standard criteria (Cheson 2007; Owen 2013). Endpoints included overall response rate (ORR), time to response, duration of response (DOR), lymph node response, progression-free survival (PFS), overall survival, and safety. The final data cutoff date was 22 Oct 2018.
Results: Of 125 patients enrolled, 15 (12%) had MZL (sMZL, n = 1; nMZL, n = 5; eMZL, n = 9) and 10 (8.0%) had LPL/WM. Median age was 65 years and most were non-Hispanic (n = 24; 96%) and White (n = 23; 92%). At diagnosis, 80% of MZL and 100% of LPL/WM patients had stage IV disease. The largest lesion at baseline was ≥5 cm for 5 (33%) MZL and 3 (30%) LPL/WM patients. Baseline median IgM level was elevated for 80% of LPL/WM patients (median 1.9, IQR 1.0-2.7 g/dL). Baseline beta2-microglobulin level was >3 µg/mL for 1 of 9 LPL/WM patients with values recorded (median 2.5 [range 1.7-3.1] µg/mL). For MZL and LPL/WM patients, 7 (47%) and 7 (70%) had ≥3 prior therapies, respectively. Common regimens for all 25 patients included rituximab-cyclophosphamide-doxorubicin-vincristine-prednisone (44%), rituximab-cyclophosphamide-vincristine-prednisone (40%), rituximab only (28%), bendamustine only (24%), and bendamustine-rituximab (20%).
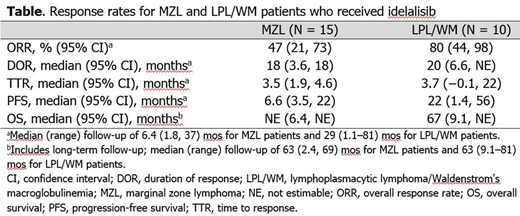
For MZL, the ORR (95% confidence interval [CI]) was 47% (21%, 73%), with median duration of therapy of 6.4 (range 1.8-37) mos. Of 7 responders, 1 had a complete response and 6 had partial responses (PR). Seven had stable disease (SD) and 1 had progressive disease (PD). Fourteen (93%) patients had reduction in lymph nodes, with 8 (53%) having ≥50% reduction in the sum of the products of the greatest perpendicular diameters (SPD). Median PFS was 6.6 (95% CI 3.5, 22) mos and median DOR was 18 (range 0-18) mos (Table).
For LPL/WM, the ORR (95% CI) was 80% (44%, 98%), with a median duration of therapy of 29 (range 6.4-51) mos. Of 8 responders, 7 had PR and 1 had a minor response. There was 1 SD and 1 PD. Nine (90%) patients had lymph node reduction, with 5 (50%) having ≥50% reduction in SPD. Median PFS was 22 (95% CI 1.4, 56) mos and median DOR was 20 (range 1.7-50) mos (Table).
All 25 patients had ≥1 treatment-emergent adverse event (TEAE), 16 (64%) had a serious AE, and 11 (44%) had dose reduced due to a TEAE. Grade ≥3 TEAEs occurred for 22 (88%) patients; neutropenia (n = 7, 28%), diarrhea (7, 28%), alanine aminotransferase increased (4, 16%), asthenia (3, 12%), and pneumonia (3, 12%) were the most frequent. All patients eventually discontinued treatment due to disease progression (14, 56%), AE (6, 24%), death (3, 12%), investigator request (1, 4%), or other (1, 4%). Ten patients have died, 3 during the study and 7 during the long-term follow-up.
Conclusions: Monotherapy with idelalisib showed high rates of antitumor activity in this small subset of patients with MZL and LPL/WM refractory to prior therapy with rituximab and an alkylating agent; prolonged disease control was achieved for LPL/WM patients. No new safety signals were identified despite longer follow-up.
Wagner-Johnston:Bayer: Membership on an entity's Board of Directors or advisory committees; Jannsen: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees; ADC Therapeutics: Membership on an entity's Board of Directors or advisory committees. Schuster:Genentech: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Patents & Royalties: Combination Therapies of CAR and PD-1 Inhibitors with royalties paid to Novartis, Research Funding; AstraZeneca: Honoraria; Pharmacyclics: Honoraria, Research Funding; Merck: Honoraria, Research Funding; Acerta: Honoraria, Research Funding; Loxo Oncology: Honoraria; Nordic Nanovector: Honoraria; Pfizer: Honoraria; AbbVie: Honoraria, Research Funding; Gilead: Honoraria, Research Funding. de Vos:Verastem: Consultancy; Portola Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Bayer: Consultancy. Salles:Epizyme: Consultancy, Honoraria; Roche, Janssen, Gilead, Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Amgen: Honoraria, Other: Educational events; BMS: Honoraria; Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Novartis, Servier, AbbVie, Karyopharm, Kite, MorphoSys: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Educational events; Autolus: Consultancy, Membership on an entity's Board of Directors or advisory committees. Jurczak:Bayer: Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding; Incyte: Research Funding; Sandoz: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novo Nordisk: Research Funding; Celtrion: Research Funding; MorphoSys: Research Funding; Gilead: Research Funding; Roche: Research Funding; Servier: Research Funding; Takeda: Research Funding; TG Therapeutics: Research Funding; Loxo: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding. Rajakumaraswamy:Gilead Sciences, Inc.: Employment. Xing:Gilead Sciences, Inc.: Employment. Gopal:Seattle Genetics, Pfizer, Janssen, Gilead, Sanofi, Spectrum, Amgen, Aptevo, BRIM bio, Acerta, I-Mab-pharma, Takeda, Compliment, Asana Bio, and Incyte.: Consultancy; Teva, Bristol-Myers Squibb, Merck, Takeda, Seattle Genetics, Pfizer, Janssen, Takeda, and Effector: Research Funding; Seattle Genetics, Pfizer, Janssen, Gilead, Sanofi, Spectrum, Amgen, Aptevo, BRIM bio, Acerta, I-Mab-pharma, Takeda, Compliment, Asana Bio, and Incyte: Honoraria.
Idelalisib is a selective oral inhibitor of PI3K-delta that has shown antitumor activity in previously treated indolent non-Hodgkins lymphomas in phase 1 and 2 studies. It is approved for treatment of relapsed follicular lymphoma that has progressed on 2 prior systemic therapies, relapsed chronic lymphocytic leukemia in combination with rituximab when rituximab alone would be considered appropriate due to other comorbidities, and relapsed small lymphocytic lymphoma that has progressed on 2 prior systemic therapies. In this presentation, we provide results of 2 less common subgroups of indolent non-Hodgkins lymphoma, Âmarginal zone lymphoma and lymphoplasmacytic lymphoma/Waldenstrom's Macroglobulinemia, Âfrom the completed phase 2 trial with long-term follow-up.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal