Introduction: Mantle cell lymphoma (MCL) is rare B-cell lymphoma subtype with usually aggressive behavior. Mutations of TP53 gene and complex karyotype (CK) were described to be poor prognostic factors (Obr A et al, 2018), but their impact on primary resistance to induction has not been investigated.
Methods: We analyzed 115 MCL patients (pts) treated in two Czech university centers from 4/2006 to 10/2016. Both classical cytogenetics and next generation sequencing (NGS, MiSeq, Illumina) for TP53 mutation detection were performed on tumoral tissue (peripheral blood, bone marrow) in all patients. Cut-off for TP53 mutation was 1% variant allele frequency (VAF). CK was defined as 3 and more cytogenetic aberrations in one cell population. Pts with stable or progressive disease (SD/PD) during induction or with relapse within 6 months after induction completion were considered as primary refractory (PrR). Variables were compared by chi-squared test. T-test was used to compare the difference between means of TP53 mutation load in PrR+ and PrR- subgroup. Cut-off for TP53 mutation load (27%) was established as median VAF. Overall and progression free survival (OS, PFS) were calculated from the date of diagnosis.
Results: The median age at diagnosis was 66 (40-87) years. Ninety-six percent of pts had advanced disease (III and IV). MIPI score was low, intermediate and high in 19.1%, 27.8% and 53.0% pts, respectively. Induction regimens used were as follows: R-CHOP/R-CHOP-like in 47.8%, intensive R-HDAC-containing in 38.3% and non-anthracycline regimen in 9.6% pts. Complete and partial response was achieved in 53.0% and 27.0% pts, resp. SD/PD was observed in 11.3% pts. Overall, 27 (23.5%) pts were considered as primary refractory. TP53 mutation and CK were present in 37 (32.3%) and 15 (13.0%) pts, respectively.
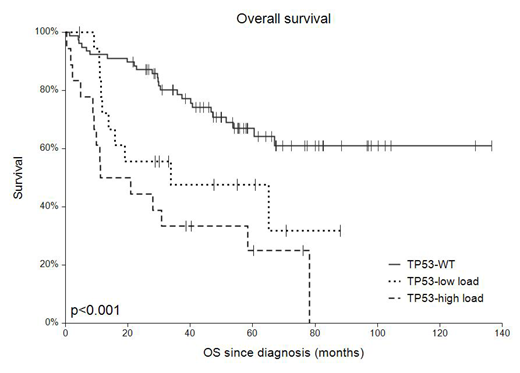
Age, disease stage, ECOG score, MIPI, HDAC therapy and CK did not correlate with PrR status. Significantly higher TP53 mutation load was observed in the PrR+ (42%), compared to PrR- subgroup (25%, p=0.03). After median follow-up of 4.6 years, 3-year overall survival (3-y OS) and 3-year progression free survival (3-y PFS) in all pts was 65.8% and 50.9%, resp. Median OS in PrR+ and PrR- pts was 9.2 months, and 4.5 years, resp. Survival analysis stratified according to the TP53 mutation status/mutation load showed 3-y OS and 3-y PFS for wild type (TP53-WT), low mutation load (TP53-low load), high mutation load (TP53-high load) 74.2%, 47.6%, 33.3% and 56.0%, 37.0%, 27.8%, respectively (p=0.001 both).
Conclusions: High TP53 mutation load (>27% VAF), but not CK, has significantly correlated with refractory disease in MCL pts. Pts with high mutation load of TP53 gene should be considered to an innovative treatment.
Acknowledgement: Supported by IGA_LF_2019_001, MH CZ - DRO (FNOl, 00098892), AZV16-32339A and AZV16-31092A grants
Trneny:Morphosys: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Gilead sciences: Consultancy, Honoraria; Takeda: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal