Introduction
The tumor immune microenvironment (TiME) of DLBCL at diagnosis bears many biomarkers known to predict sensitivity to checkpoint blockade therapy (CBT). Approximately 25% of DLBCL, harboring PDL1 gene alteration, exhibit an immune inflamed phenotype. However, CBT studies in relapsed DLBCL show very low response rates.
The immune landscape of DLBCL in the setting of relapse has not yet been characterized. We hypothesized that the TiME can be influenced by the therapy, explaining the CBT lack of efficacy. We explored the TiME evolution by comparing the tumor infiltrating lymphocytes (TIL) and the immune evasion signature by protein and gene expression (GE) in paired biopsies of DLBCL at diagnosis and at relapse.
Method
This study included patients with DLBCL treated with first-line R-CHOP-like regimen, in which we had access to nodal biopsies obtained pre-treatment and at relapse.
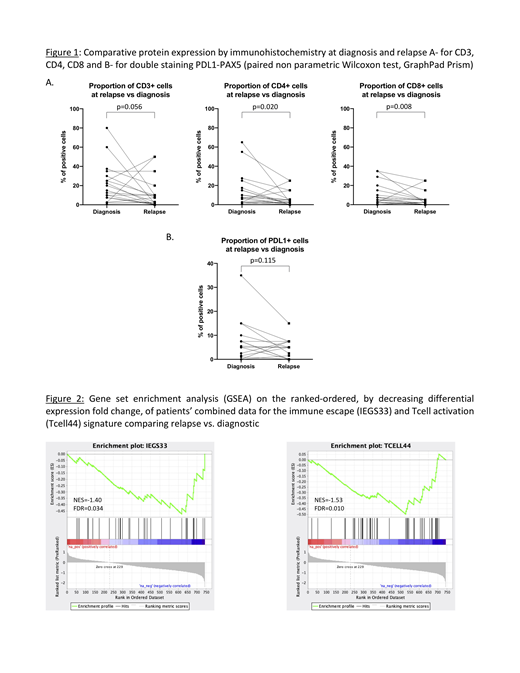
Assessment of TIL and PDL1+ cell content was carried out by CD3, CD4, CD8 immunostaining and with PDL1 (Ventana, SP263) and PAX5 double staining. These were performed on formalin-fixed, paraffin-embedded (FFPE) tissue sections cut at 4µm. The proportion of each cell-type was expressed in relation to total nucleated cells. PDL1+ cell proportion was expressed for both total cells and tumor cells. The paired non-parametric Wilcoxon test, double-sided with p=0.05, was used for comparison.
GE using a panel of 760 cancer immune genes was performed with the digital hybridization NanoString platform on paired FFPE specimens. NSolver software was used for normalization on housekeeping genes, differential expression (DE) and cell-type profiling. The correlation between IHC and GE variation were computed using the Spearman test. Analysis of enriched pathways on combined patient data were performed with GSEA software, using two gene sets for T-cell activation and immune evasion validated in B-cell lymphoma, and Ingenuity Pathway Analysis (IPA) for the 339 highest changed genes. The pathway enrichment analysis was reported for false discovery rate (FDR) <0.05.
Results
Twenty DLBCL patients with paired diagnostic and relapse biopsies were studied. IHC was performed on 19 patients (necrotic tissue for one patient) and GE by NanoString on 6 patients. The median number of treatments received prior to obtaining the relapsed biopsy was 3 (1-6). Three patients had prior exposure to CBT, none from the patients in whom GE was performed. Our population was composed of 2/3 germinal center B-cell (GCB) DLBCL. Six patients had transformed DLBCL.
At relapse, CD4 and CD8 cells density was significantly reduced compared to diagnosis. The median percentages of CD3, CD4 and CD8 were 15%, 7.5% and 5% at diagnosis and 7.5%, 2.5% and 2.5% at relapse, respectively (Figure 1A). The median proportion of PDL1+ cells (n=15) did not differ at relapse compared to pre-treatment (5.25% and 5%, respectively) (Figure 1B). At diagnosis, 87% of biopsies were found to be positive for PDL1 (≥1% of positive cells) and 73% at relapse. The PDL1 positive cells were mostly immune cells; only 3 samples had tumor cells expressing PDL1 at pre-treatment and 4 at relapse with <1% of positive tumor cells in all cases.
The GE profile detected 63 genes that were significantly different in relapse vs pre-treatment samples (p<0.005), including 8 up-regulated and 55 down-regulated. The correlation for T-cell abundance variation between IHC and GE was high (r=0.94, p=0.017). For the subset of 6 patients in whom GE was performed, the T-cells were not significantly reduced as measured by both IHC and GE. However, the GSEA for immune escape genes and T-cell activation signatures were both down-regulated (FDR=0.033 and 0.010, respectively) (Figure 2). IPA predicted decreased activation of leukocytes (z-score=-6.317) and Th2 activation pathway (z-score=-3.182).
Conclusion
At relapse, a proportion of DLBCL have a significant reduction in T cell infiltration. As well, they acquire a non-T cell-inflamed TiME. The T-cell inhibition seems to be independent of local T-cell immunoregulatory mechanisms as the immune escape signature is also reduced. This non immunogenic, "cold" condition could explain the lack of efficacy of CBT in the relapsed setting. Prior exposure to steroid containing therapy might be a trigger for intra-tumor T-cell desertion and downregulation. This observation must be confirmed on a larger population. Further analyses will be presented.
Johnson:BD Biosciences: Other: Provided a significant proportion of the antibodies used in this project free of cost.; Lundbeck: Employment, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel fees, gifts, and others, Research Funding; Seattle Genetics: Honoraria; Merck: Consultancy, Honoraria; Roche: Consultancy, Employment, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel fees, gifts, and others, Research Funding; BMS: Consultancy, Honoraria; Abbvie: Consultancy, Employment, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Assouline:Janssen: Consultancy, Honoraria, Speakers Bureau; F. Hoffmann-La Roche Ltd: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria, Speakers Bureau; Abbvie: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal