Introduction
Mature B-cell lymphoma (MBL) accounts for approximately 60% of all non-Hodgkin lymphoma (NHL) in children and adolescents (Cairo et al, Blood, 2007). MBL in children and adolescents is comprised of approximately 75-80% Burkitt lymphoma (BL), 15-20% diffuse large B cell lymphoma (DLBCL) and 1-2% primary mediastinal B-cell lymphoma (PMBL). However, despite the differences in histology they are treated uniformly in children and adolescents (Cairo, BJH, 2016). The use of short and intense multiagent chemotherapy alone and in combination with rituximab (R) results in ≥90% event-free survival (EFS) in children and adolescents with BL and DLBCL (Cairo et al, JCO, 2012; Goldman/Cairo Leukemia, 2013; BJH, 2014). However, similar chemotherapy approaches in adolescents and young adults with PMBL have only resulted in a 60-70% EFS (Gerrard/Cairo et al, Blood, 2013). Furthermore, patients with induction failure, recurrent or refractory MBL have a dismal prognosis with ≤30% overall survival (OS) with current re-induction platforms and autologous stem cell transplantation (Cairo et al, BJH, 2018). Newer therapeutic strategies are urgently needed for recurrent/refractory patients with MBL, especially those with the BL subtype and newly diagnosed and refractory patients with PMBL (Cairo, BJH, 2019). We previously demonstrated that Obinutuzumab (O), a new type II anti-CD20 monoclonal antibody, is an active agent against both BL and PMBL (Awasthi/Cairo et al, BJH, 2015). Additionally, we have previously demonstrated high expression of CD79b in children and adolescents with BL and PMBL (Miles/Cairo et al, BJH 2007). Polatuzumab vedotin (PV), an anti-CD79b antibody-drug conjugate, recently approved by the FDA in adults with recurrent/refractory DLBCL has been demonstrated to be an active agent alone and in combination with chemotherapy in all molecular forms of adult DLBCL (Pfeifer et al, Leukemia, 2015; Corrinna et al, Lancet Oncology, 2015; Morschauser et al, Lancet Onc, 2019; Tilly et al, Lancet Onc, 2019). However, the efficacy of PV alone or in combination with R or O against other subtypes of B-NHL, including BL and PMBL, is relatively unknown.
Objective
To determine the in-vitro cytotoxicity and changes in in-vivo survival in a BL NSG xenograft model of PV alone or in combination with O vs R against R-sensitive and R-resistant BL and PMBL.
Methods
We compared the cytotoxicity of PV±R (10 ug/ml) vs PV±O (10 ug/ml) against R-sensitive BL (Raji) and R-resistant BL (Raji 4RH) and PBML (Karpas-1106p) alone or with ex-vivo expanded NK cells (Chu/Cairo et al, Can Imm Res, 2015) (10:1 E:T) by the DELFIA cytotoxicity assay. PV and O were generously supplied by Genentech and Roche, respectively. Furthermore, NSG mice (NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ) were xenografted with luciferase positive BL (Raji, Raji 4RH) and PMBL cells (Karpas-1106p) and treated with PV (5 mg/kg) + O (20 mg/kg) vs PV + R (20 mg/kg) vs PV vs IgG isotype control vs PV + O + NK vs PV + R + NK vs PV + NK vs O + NK vs R + NK vs PBS (without tumor) and tumor burden was compared between treatment groups using the IVIS bioluminescence system and probability of OS by KM method as we have previously described (Chu/Cairo et al, Can Imm Res, 2015).
Results
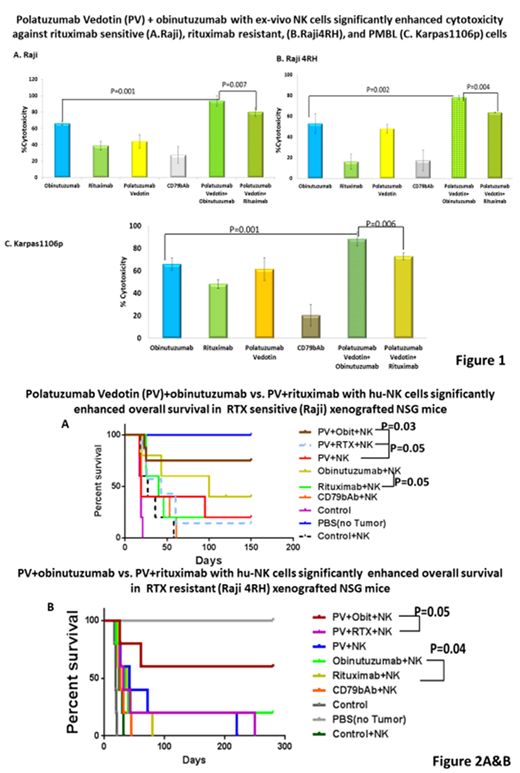
PV + O + NK induced significantly more in-vitro cytotoxicity against BL Raji compared to PV + R + NK (p<0.007) vs PV, R or O + NK (p<0.0001), BL (Raji 4RH [R-resistant BL]) PV + O vs PV + R (p<0.004) and O, R or PV (p<0.002) and against PMBL (Karpas-1106p) PV + O + NK vs PV + R + NK (p<0.006) vs O, R, or PV + NK (p<0.001) (Fig. 1A, 1B, 1C, respectively). Most importantly, PV + O + NK vs PV + R + NK vs PV + NK + IgG isotype control significantly enhanced probability of survival in BL (Raji) and BL (Raji 4RH) NSG xenografts (p<0.03 and (p<0.05), (95.5 vs 50.4 days) (185 vs 47 days), respectively (Fig. 2A and 2B, respectively).
Conclusions
PV alone and in combination with O significantly induces cytotoxicity against BL, R-resistant BL and PMBL. Most importantly, PV + O + NK cells result in a significantly improved OS in BL and R-resistant BL NSG xenografts. These preclinical results suggest that PV should be considered for investigation in patients with both recurrent/refractory BL and PMBL and in patients with newly diagnosed disease with either high risk features or those with poor responses to induction therapy.
Authors AA, MB & AA are all considered co-primary first authors
Klein:Roche: Employment, Equity Ownership, Patents & Royalties. Cairo:Jazz Pharmaceuticals: Other: Advisory Board, Research Funding, Speakers Bureau; Osuka: Research Funding; Miltenyi: Other: MTA.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal