Introduction.
Elderly patients aged 65 or older with acute myeloid leukemia (AML) are often ineligible for hematopoietic stem cell transplantation (HSCT) and generally have a poor prognosis. The prognostic risk classification based on NCCN Guidelines Version3. 2017; NCCN 2017 (O'Donnell MR, JNCCN. 2017) is widely performed; however, the impact of this classification on the prognosis of such elderly AML patients is unclear. While nutritional status assessment using controlling nutritional status (CONUT score) based on serum level of albumin (Alb), total-cholesterol (T-chol) and total lymphocyte count (TLC) predicts prognosis of elderly patients with solid tumor (Liu X, BMC Cancer. 2018), the prognostic significance of nutritional status in elderly patients with AML remains to be clarified.
Methods.
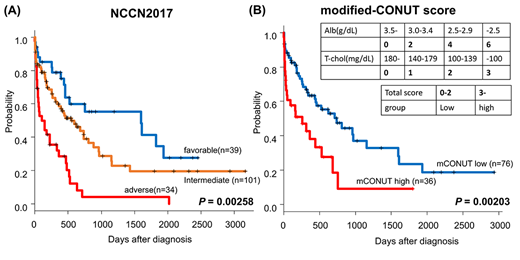
Hokkaido Leukemia Net (HLN) is prospective cohort study collecting AML samples from hospitals of North Japan Hematology Study Group (NJHSG). In this study, we focused on newly diagnosed AML patients aged 65 or older treated without HSCT, and investigated cytogenetic and molecular abnormality of leukemic cells including FLT3-ITD, NPM1, CEBPA, and KIT. We stratified the patients into favorable, intermediate, and adverse risk group based on NCCN 2017. In order to adjust the assessment of nutritional status for hematopoietic malignancy, we modified the CONUT score eliminating TLC from evaluation criteria (modified-CONUT score, Table) and defined patients with score 3 or more at diagnosis as high group. We evaluated the impacts of NCCN 2017 and modified-CONUT scores on overall survival (OS) in these patients. The study procedures were in accordance with the Helsinki Declaration and institutional ethical guidelines, conducted under the auspices of the institutional ethics committee, and approved by the institutional review boards.
Results.
Overall, 181 patients with newly diagnosed AML patients aged 65 or older enrolled in HLN between April 2010 and March 2018. Seven patients undergone HSCT were excluded and 174 patients were reviewed (Age 65-93, median 71; male 104, female 70). In this cohort, classification based on NCCN 2017 successfully divided the prognosis of the patients for 2-year and 5-year OS [2-year OS; favorable group, 59.9%; intermediate group, 43.8%; adverse group, 8.1%, 5-year OS; favorable group, 41.5%, intermediate group, 19.7%; adverse group, 4.1%, P=0.00258, Figure A]. On 112 patients who had available records of serum Alb levels and T-chol levels at diagnosis, OS in patients with high modified-CONUT score was significantly lower than the low score group [2-year OS; low score group, 50.3%; high score group, 18.5%; 5-year OS; low score group, 23.5%; high score group, 9.24%, P=0.00203, Figure B]. In a univariate analysis, adverse group in NCCN 2017 and high modified-CONUT score were associated with poor 2-year OS. A multivariate analysis demonstrated that adverse group in NCCN 2017 and high modified-CONUT score were independently associated with poor 2-year OS (adverse group in NCCN 2017; HR, 2.464 ; 95% CI, 1.514 to 4.012, P=0.0002854, high modified-CONUT score; HR, 1.664 ; 95% CI, 1.051 to 2.635, P=0.02976; log-rank). Altogether, we demonstrated that risk stratification based on NCCN 2017 and modified-CONUT score are both effective for predicting prognosis in elderly patients with newly diagnosed AML.
Conclusion.
The prognostic risk classification based on AML disease status using NCCN Guidelines 2017 effectively stratify prognosis of elderly patients with AML. Moreover, new assessment scoring of patients' nutrition status based on modified-CONUT score can easily stratify elderly patients with newly diagnosed AML.
Teshima:Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal