Background: The presence of FLT3 "internal tandem duplication" (FLT3-ITD) mutation is associated with poor prognosis in acute myeloid leukemia (AML). However, the concomitant presence of NPM1 mutation (NPM1-mut) partially overcomes the negative prognostic impact of FLT3-ITD, which is also modulated by FLT3-ITD/wild-type allelic ratio. NPM1 and FLT3 mutational status assessment is strongly recommended for risk stratificationat diagnosis by the last European Leukemia Net (ELN) guidelines.
Aims: To investigate the efficacy of an intensive fludarabine-containing induction regimen (FLAI) for fit, de novo AML patients according to NPM1 and FLT3-ITD mutational status.
Methods: One-hundred and sixteen consecutive AML patients, treated in 3 Hematology Italian centers from January 2008 to January 2018, were included in this analysis. Twenty five patients showed isolated FLT3-ITD, 39 concomitant FLT3-ITD and NPM1-mutation and 52 isolated NPM-1-mutation.Median age was 52 yrs (range: 18-65 years). All patients received fludarabine, high dose cytarabine-based induction (fludarabine 30 mg/sqm and ARA-C 2g/sqm ondays 1 to 5 plus idarubicin 10 mg/sqm on days 1-3-5). For patients achieving CR fludarabine was omitted on II induction course and idarubicin dose was increased to 12 mg/sqm. Before2017 patients with isolated FLT3-ITD mutation were scheduled to receive allogeneic bone marrow transplantation (BMT) in first complete remission regardless of allelic burden whereas after 2017 only patients with high allelic burden received BMT in 1st CR. Minimal residual disease was evaluated on marrow samples using multicolor flow-cytometry (MFC)or NPM1 expression levels. Negative MFC-MRD wasdefined by the presence of less than 25 clustered leukemic cells/105 total events (threshold of 0.025% residual leukemic cells, Minetto et. al, BJH 2019). NPM1mutation (NPM1-A, B and D) was measured using Muta Quant Kit Ipsogen from Qiagen. FLT3-ITD allelic burden was available in31/64 of FLT3-ITD patients.
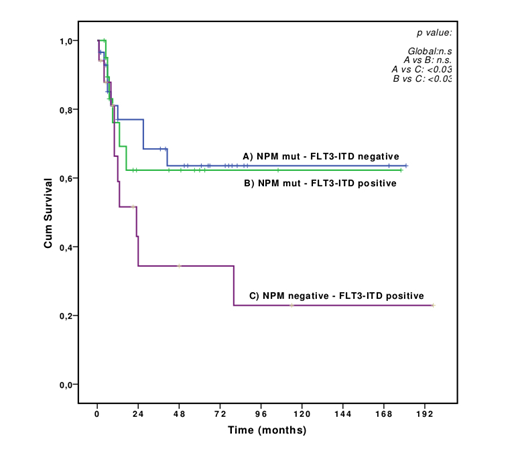
Results: Overall 60-days mortality was 4%. After two induction cycles, 101 patients achieved CR (87%). Thirty-three/101 (33%) CR patients underwent BMT in first CR. After a median follow up of 61 months, 3-year overall survival (OS) was 56.8% (median not reached). In univariate analysis OS duration was favorably affected by age <55 yrs (p<0.05), MRD-negative status after induction (both MFC and NPM1 based MRD) (p<0.001) and wild-type FLT3(p<0.05). However, in multivariate analysis only MRD status significantly affected OS (p<0.003). The probability of achieving a molecular MRD negative CR after first cycle among NPM1-mut patients was similar between patients with or without concomitant FLT3-ITD mutation (61% and 66%, respectively, p=n.s.). Interestingly, in younger patients (< 55yrs) OS was comparable in case of isolated NPM1 mutation or concomitant NPM1/FLT3-ITD mutation (3-year OS 68.4% and 62.3%, respectively, p= n.s, Figure 1), regardless of FLT3-ITD allelic burden.Patients with isolated FLT3-ITD mutation had a significantly worse prognosis (3-year OS 34.4%, p<0.05). Again, multivariate analysis showed that persistence of MRD (by any method, p <0.05) was the strongest predictor of outcome. Moreover, performing BMT infirst CR did not impact OS neither in univariate or multivariate analysis.
Conclusion: Despite the potential bias due to the retrospective nature of the analysis, our data indicate that intensive fludarabine-high dose cytarabine-based induction exerts a strong anti-leukemic efficacy in younger AML patients carrying NPM1 mutation irrespectively of FLT3 mutational status.Thus, the synergism of fludarabine and cytarabine seems to affect the intrinsic chemosensitivity of NPM1-mut leukemic cells, overcoming the negative impact of FLT3-ITD. Moreover, our data suggest the strong prognostic impact on survival of MRD clearance and question the role of BMT in I CR in this setting of patients.
Candoni:Gilead: Honoraria, Speakers Bureau; Celgene: Honoraria; Pfizer: Honoraria; Janssen: Honoraria; Merck SD: Honoraria, Speakers Bureau. Bocchia:Incyte: Honoraria; Novartis: Honoraria; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal