Background: Transfusion is a major therapeutic of sickle cell disease (SCD); however, DHTR is one of the most feared complications . Prevention of allo immunization, by extended RBC matching is insufficient to prevent all cases of DHTR. Therefore, B cell depletion therapy should be also useful, especially in previously immunized patients to avoid the emergence of new allo-antibodies. Rituximab (RTX) is used for preventing alloimmunization for patients with a history of DHTR. Therefore, secondary prevention with rituximab prior a new exposure to transfused RBCs could be a relevant option. Here, we will report our experiences of RTX use in SCD adult patients with a previous history of DHTR.
Methods: In this retrospective observational study, the data from 58 consecutive RTX infusion in 44 SCD patients with history of DHTR in our French referral center for SCD were analysed. Medical, biological and blood bank records of patients, clinical signs, rate of hemoglobin A (HbA) after transfusion (TF) were collected. To evaluate the persistence of transfused RBCs, the DHTR risk probability on days 15 and 30 after TF was evaluated according to Mekontso Dessaps nomogram. We also reported serious adverse events like infections in the year after RTX infusion. In cases of programmed surgery, 1 gramme of RTX was administred at day 1 and 15 few weeks before or one injection in emergency situation, with low dose of steroides. Adjuvant measure to avoid transfusion like EPO, Iron injection and hydroxyurea was decided in some cases.
Results: We analyzed 58 cases of RTX administered to 44 adult patients with SCD, 10 of whom received two or more times this drug. A transfusion (TF) was required in 33/58 cases (56%). We distinguished three groups of patients. In the first group of 21 cases (36%), rituximab was used preventively before planned surgery at risk of bleeding, only 8 cases were transfused. In the second group of 30 cases (53%) during an acute event, in 19 cases patients received a transfusion. The third group of 7 patients received RTX during an active DHTR with hyperhemolysis requiring transfusion to protect an imminent transfusion and finally 6 of them was transfused.
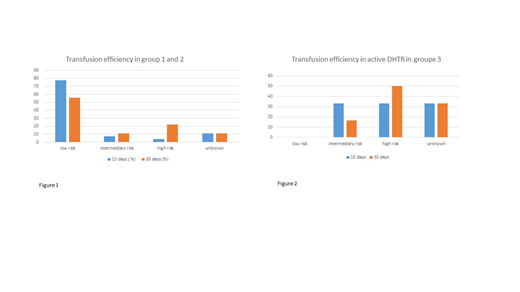
To evaluate the efficacy of transfusion we analyzed group 1 and 2 together and separately the third group with active DHTR and hyperhemolysis. In the first and second groups, HbA measurements was not available or interpretable in 11,1% of cases. On day 15 after TF, 77,8% of cases were classified as having a low probability of hemolysis, 7.4 % as intermediate probability and 3.7% as high probability. On day 30 after TF: 55,6% were into the low probability of hemolysis subgroup, 11,1% in the intermediate probability and 22,2% in the high probability group. (Figure 1) In group 3, HbA measurement wasn't available in 2 cases. On day 15 after TF, no cases were classified as having a low probability of hemolysis, 33,3 % as intermediate probability and 33.3% as high probability. On day 30 after TF: 33,3% were in the intermediate probability and 50 % in the high probability group. (Figure 2)
Infection requiring intravenous antibiotic were observed in 19 cases/58 (32.7%) with a bacterial documentation in 73,7 %. In 63% of these cases, patients have been hospitalized in intensive care unit for acute events before RTX administration and had other risk factors of infection. The median time of apparition of infection was 28 days [11.5-46.5]. We report 4 deaths (6,8%), two patient died due to a hyperhemolysis syndrome with multiorgan failure that started before RTX administration, two other were due to an end stage cancer. These deaths are not related to the use of RTX.
Conclusion: This study suggests that RTX can be safely used for preventing DHTR in patients with a previous history of DHTR and detected antibodies. We show that transfusion efficiency at day 15 post TF is better than days 30 postTF. The effectiveness of TF in active DHTR with h yperhemolysis is much lower, as most patients lose the transfused units at day 30 post TF.Beyond the use of RTX, the use of other measures such as hydroxyurea and erythropoietin to avoid the need of transfusion in these patients must be emphasized.
Infection risk after RTX therapy is difficult to assess. In most cases an active inflammatory event was in process. Additional prospective studies are needed to improve the management of this challenging clinical situation.
Michel:Novartis: Consultancy; Amgen: Consultancy; Rigel: Consultancy. Galactéros:Addmedica: Membership on an entity's Board of Directors or advisory committees. Bartolucci:Novartis: Membership on an entity's Board of Directors or advisory committees; AddMedica: Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; HEMANEXT: Membership on an entity's Board of Directors or advisory committees; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal