Background
During pregnancy, women develop a physiologic hypercoagulable state related to hormonal changes and physical factors which can predispose them to the development of venous thromboembolism (VTE). Anticoagulation may be prescribed for underlying conditions that add additional risk of developing a thromboembolism during pregnancy or to minimize the risk of pregnancy loss. Heparin and low molecular weight heparin are believed to be safe to use during pregnancy, however these agents do present potential risks, particularly of bleeding for both the mother and fetus. Examination of the clinical outcomes, specifically bleeding and transfusion requirements at the time of delivery and the immediate postpartum period, in patients taking enoxaparin or heparin during high-risk pregnancies can provide further information on the safety of anticoagulants in pregnancy.
Methods
We conducted a retrospective case-control analysis of patients admitted to Georgetown University Hospital (GUH) for labor and delivery from the maternal fetal medicine service taking anticoagulation ante- and postpartum (N=13) as compared to matched controls (N=26) from January 2016 through December 2017. Individuals were matched for age (+/- 2 years), delivery date (+/- 1 month), delivery method (Cesarean or Vaginal), and gravidity. Women who underwent supplemental surgical procedures during delivery, with exception of tubal ligation, were excluded. Means independent t-tests were utilized to determine if women taking anticoagulants during pregnancy were more likely than matched controls to have increased estimated blood losses (EBL), blood transfusion requirements, or changes in antepartum hemoglobin (Hgb) or hematocrit Hct) (≤48 hours prior to delivery) verses postpartum (≤48 hours after delivery). Results with p < 0.05 were deemed significant.
Results
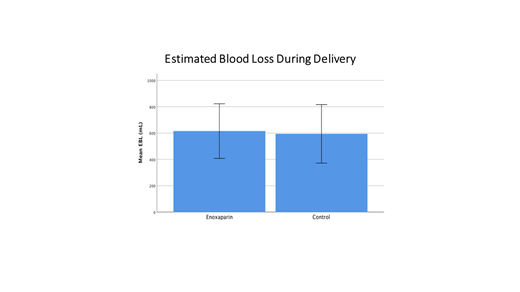
There was no significant difference in EBL between individuals taking anticoagulants during pregnancy as compared to controls (615.37mL vs 594.23 mL, p = 0.064). There was also no significant difference between antepartum Hgb or Hct (11.76 g/dL vs11.92 g/dL, p = 0.358 and34.99% vs 35.70%, p = 0.766, respectively), or postpartum Hgb or Hct (10.13 g/dL vs10.16 g/dL, p = 0.959 and 30.465vs30.57%, p = 0.338, respectively). Furthermore, the difference in Hgb or Hct before delivery to immediately after was not statistically significant (1.63 g/dL vs 1.76 g/dL, p = 0.056 and 4.53% vs5.13% p = 0.236, respectively) between the two groups. Interestingly, the mean number of units of RBCs transfused was significantly higher for patients on Enoxaparin as compared to controls (0.77 units vs 0.00 units respectively, p = 0.003), however only one patient in the Enoxaparin group required transfusions.
Conclusion
These data suggest that anticoagulation during high-risk pregnancies is not associated with an increased estimated blood loss or significant reduction in postpartum Hgb and Hct. Although an overall mean increase in units of blood transfused was noted for the anticoagulation group this was based on one patient and may not be representative. Although these results are reassuring that there are minimal risks to anticoagulation in a high risk maternal fetal medicine population additional analyses should be completed from a larger patient population.
Broome:Sanofi Genzyme: Honoraria, Research Funding; Rigel: Research Funding; Cellphire: Research Funding; Alexion: Honoraria, Research Funding; Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal